RESEARCH ARTICLE
- Shruti Mony MD 1
- Annie TophamMD 2
- Jiteshwar Singh Pannu MD* 3
- Ambuj Kumar MD, MPH 4
- Seth Felder MD 5
- Jason Klapman MD6 6
1Department of Gastroenterology, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma.
2Department of Medicine, University of South Florida, Tampa, Florida.
*3Department of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, Oklahoma.
4Department of Biostatistics and Research, University of South Florida, Tampa, Florida.
5Department of Colorectal Surgery, Moffitt Cancer Center, Tampa, Florida.
6Department of Gastroenterology, Moffit Cancer Center, Tampa, Florida
*Corresponding Author: Jiteshwar Singh Pannu MD* 3
Citation:
Jiteshwar Singh Pannu MD*3, (2024), Variability in Endoscopic Tattoo Practices Among Colorectal Surgeons and Gastroenterologists:
A Nationwide Survey, Digestive System and Hepatobiliary Diseases (DSHD)1(1), DOI: https://doi.org/10.64347/3066-3040/DSHD.002
Copyright: © (2024), Jiteshwar Singh Pannu MD*3, this is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: January 09, 2024 | Accepted: February 16, 2024 | Published: March 27, 2024
Abstract
Background:
Endoscopic tattooing is a crucial surgical landmark for colorectal neoplasms prior to operative resection. Despite widespread use, no established endoscopic tattooing guidelines exist for optimal location or technique. We aimed to study the practices among gastroenterologists (GI) and colorectal surgeons (CRS).
Methods:
A national, electronic, anonymous survey was sent to program directors of adult GI and CRS residencies in the US. 108 were completed and analyzed. Descriptive statistics was used to summarize demographic and response variables. The difference in response rates between groups was assessed using the Fisher exact test and summarized as odds ratio with 95% confidence intervals (CI) and 2-tailed statistical significance.
Results:
Of 108 physicians who responded to the survey, 86% reported tattooing suspected colorectal cancer lesions: GI (68 of 78, 87.2%) and CRS (25 of 30, 83.3%). GI tattoo proximal and distal to the lesion (57.7%) compared to CRS who tattoo 2- 3cm distal to the lesion (76.7%), which was statistically significant (p <0.001, OR =9.52, CI=3.6-25.5). This remained unchanged when corrected for practice setting, age, gender and training. A minority tattoo cecal lesions—18.0% of GI and 23.3% of CRS. Rectal lesions were tattooed by GI 39.7% and 73.3% for CRS. For tattoo injection technique, most reported injecting while withdrawing the needle (80.8% of GI and 73.3% of CRS, p=0.227), rather than while advancing the needle. Most reported placing 2-3 marks at tattoo site (72.2%).
Conclusion:
There is wide variability of endoscopic tattooing practices between GI and CRS. Improvements in training and societal guidelines are needed to standardize practices
Keywords: Endoscopic tattooing, colorectal cancer, gastroenterologists, colorectal surgeons
Introduction:
Endoscopic localization by tattooing is an essential tool in aiding the surgical localization of suspected and proven malignant colorectal lesions for eventual surgical removal, especially minimally invasive (laparoscopic or robotic-assisted) resections [1, 2]. Relying solely on preoperative colonoscopy without use of endoscopic marking for localization of malignant lesions has been found to be inaccurate and can lead to inappropriate segments or excessive amount of bowel being removed, with the potential to miss the malignant lesion [1].
The National Comprehensive Cancer Network (NCCN) guidelines recommend the consideration of minimally invasive surgery (MIS) for colon cancer that is not locally advanced, and is not causing obstruction or perforation [3]. MIS often results in improved short-term outcomes compared to open surgery, thus is increasingly utilized as an alternative to open colectomy [4]. MIS relies on a distally placed tattoo as a visual landmark to plan the distal resection margin, since tactile feedback is limited and smaller tumors may not be readily apparent [5]. Endoscopic tattooing can accurately localize lesions [6-8], supplanting other methods of lesion localization such as placement of metallic clips or descriptive measurement from the anal verge. [8]. Tattoo provides direct visualization of the lesion site without relying solely on the endoscopic report, which at times can be inexact [9, 10]. In addition, the technique of tattoo application is critical, since incorrect injection may result in intraoperative non-visualization [3]. When this occurs either an intraoperative colonoscopy or conversion to open colectomy may be required for localization of the lesion increasing intraoperative time and potentially altering the surgical plan [5].
Despite widespread use, no established endoscopic tattooing guidelines exist in the United States regarding the optimal tattoo technique or placement relative to a particular colorectal lesion. This study aims to clarify current US practices among gastroenterologists (GI) and colorectal surgeons (CRS).
Materials And Methods:
1.Survey Design, Data Collection, and Analysis
Participation in the survey was offered to program directors of gastroenterology and colorectal surgery programs in the United States via e-mail invitation, with additional distribution to their fellows and colleagues. Programs in the American College of Gastroenterology and American Board of Colon and Rectal Surgery directories were included. We designated appropriate location for tattooing of suspected lesions to be 2-3 cm distal to the lesion.
2.Survey
- An anonymous 13 item multiple-choice survey was electronically sent and data automatically captured using RedCap software (Table 1)
| 1.State of practice |
| 2.Respondent age |
| 3.Respondent gender |
4.Respondent specialty a.Colorectal Surgery b.Gastroenterology |
Level of training a.Attending Time in practice <5>10 year b.Gastroenterology fellow Post Graduate Year 4, 5, or 6 c.Advanced Endoscopy fellowd. d.Colorectal surgery fellow |
6.Practice setting a.Academic b.Private c.Mixed |
7.Location of tattoo placement for a suspected colon cancer mass a.2-3 cm proximal to the site of the lesion b.2-3cm distal to the site of the lesion c.Within the lesion d.Both proximal and distal to the lesion |
8.Number of tattoo marks placed for a single colon cancer lesion a.One b.Two c.Three d.Four e.Greater than 4 |
9.Technique for tattooing a.Advance needle and inject as the needle is withdrawn to find submucosal space b.Inject as you advance the needle through the mucosa to find the submucosal space
|
| 10.Do you tattoo cecal lesions |
| 11.Do you tattoo rectal lesions |
12.Location of tattoo placement for cecal lesions a.Proximal to the lesion b.Distal to the lesion |
13.Location of tattoo placement for rectal lesions a.Proximal to the lesion b.Distal to the lesion |
14.Endoscopy report documentation a.Tattoo presence b.Tattoo site relative to lesion c.Number of tattoo marks placed |
Demographic information such as age, sex, specialty, practice setting and time in practice were collected. The remaining questions focused on determining tattooing practices including lesions tattooed, location of tattoo placement, and technique of tattoo injection.
Survey design included closed-ended, multiple choice questions with the ability to provide additional comments via free-text for ease of categorization. An answer to all questions was required for submission of the survey.
The primary outcome of the study was to determine if there was significant variability in endoscopic tattooing location and injection technique between gastroenterologists and colorectal surgeons. The secondary outcomes included assessing tattooing practices at specific locations (cecum, rectum) and variability of practices within each group.
3.Data Analysis and Statistics
Descriptive statistics was used to summarize demographic and response variables. The difference in response rates for all questions across the compared groups of gastroenterologists and colorectal surgeons was assessed using the Fisher exact test and summarized as odds ratio along with 95% confidence intervals (CI). The statistical significance was set at 5% and were 2 tailed. All analysis was performed using the SPSS version 26 statistical analysis package.
Results:
1.Participant Characteristics:
Of 250 invitations sent, 108 physicians completed the survey. There were more gastroenterologists (72.2%) who participated in the survey. Among the gastroenterologists, 50% were trainees and the remainder were attendings. Among the colorectal surgeons, 10% were trainees and 90% were attendings. There were varying experience levels between attendings with 24.2% in practice for less than five years, 31.8% in practice for five to ten years, and 43.9% in practice for more than ten years. The majority of gastroenterology and colorectal surgery respondents practiced in an academic setting (78.2% and 56.7% respectively) followed by mixed setting (12.8% and 33.3% respectively) and private (9.0% and 10.0% respectively) (Table 2).
Gastroenterologists (n= 78) | Colorectal Surgeons(n=30) | P value | |
Male
| 54(69.2%) | 21 (70.0%) | 0.567 |
| female | 24 (30.8%) | 9 (30.0%) | |
| Attending | 39 (50.0%) | 27 (90.0%) | |
| 14 (35.9%) | 2 (7.4%) | 0.010 |
| 8 (20.5%) | 13 (48.1%) | |
| 17 (43.6%) | 12 (44.4%) | |
| Trainees | 39 (50.0%) | 3 (10.0%) | <0> |
Practice Setting
|
61 (78.2%)
7 (9.0%)
10 (12.8%) |
17 (56.7%)
3 (10.0%)
10 (33.3%) |
0.042 |
2.Endoscopic Tattooing:
2.1. Tattoo Localization
The majority of physicians (86.1%) use endoscopic tattooing to mark suspected colorectal cancers for operative localization (Gastroenterology, 87.2%; colorectal surgery, 83.3%). There was a statistically significant difference between gastroenterologists and colorectal surgeons for tattoo location (p<0 OR =9.5, CI =3.55-25.56)>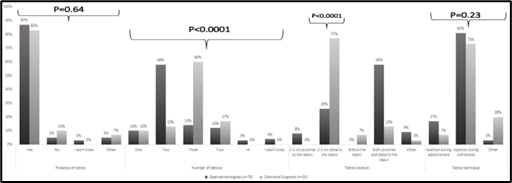
Fig 1. Comparison of Gastroenterologists and Colorectal Surgeons using standard tattooing techniqueand location
95.4% reported documenting the presence of a tattoo in their endoscopy report, 94.4% included the location of the tattoo, and 65.7% included the number of tattoos placed.
2.2Tattoo Technique
The majority of physicians in both specialties reported injecting tattoo while withdrawing the needle (80.8% of gastroenterologists and 73.3% of colorectal surgeons), rather than while advancing the needle (16.7% and 13.3% respectively). There was no statistical significance on tattoo technique. Most reported injecting two to three marks (72.2% of physicians), however 10.2% place only one mark and 14.9% place four or more (Figure 1) (Figure 2).
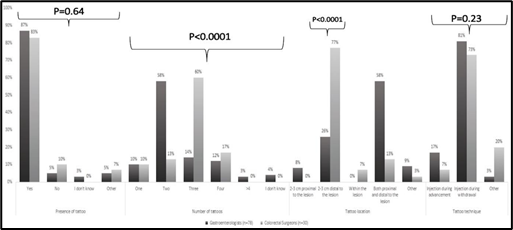
Fig1.Comparison of Gastroenterologists and Colorectal Surgeons using standard tattooing technique and location
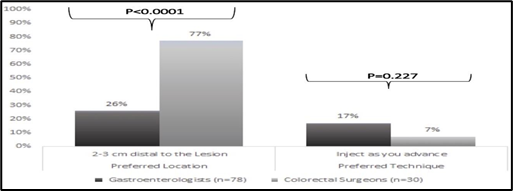
Fig 2. Comparison of Gastroenterologists and Colorectal Surgeons Regarding Endoscopic Tattooing Practices
2.3 Tattoo for Cecal and Rectal Lesions
The majority do not tattoo cecal lesions—76.9% of gastroenterologists and 73.3% of colorectal surgeons. Of the respondents that tattooed cecal lesions, 71.4% did so distally rather than proximally (19.0%). Rectal lesion tattooing was inconsistent, 39.7% of gastroenterologists tattooed compared to 73.3% of colorectal surgeons. Colorectal surgeons predominantly tattooed distal to the rectal lesion (87.5%) compared to gastroenterologists who do so proximally (46.9%) and distally (37.5%) (Figure 3) (Figure 4).
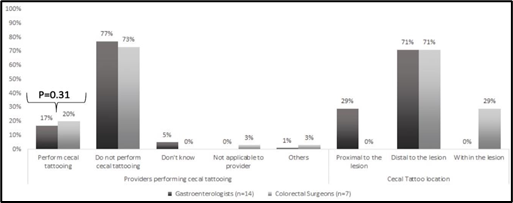
Fig 3. Comparison of Gastroenterologists and Colorectal Surgeons Regarding Endoscopic Cecal Tattooing Practices.
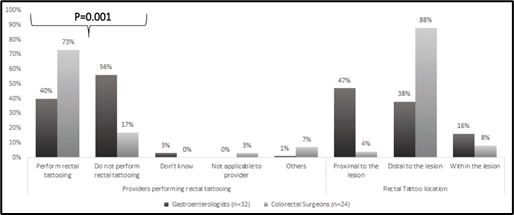
Fig 4. Comparison of Gastroenterologists and Colorectal Surgeons Regarding Endoscopic Rectal Tattooing Practices
Discussion:
Endoscopic tattooing has been in use as a method to localize colorectal lesions for over forty years. The European Society of Gastrointestinal Endoscopy (ESGE), recommends the use of endoscopic tattooing for future detection of known or suspected malignant lesions. Despite it being a widely accepted practice, there are no established guidelines regarding optimal location or technique of endoscopic tattooing in the United States, causing wide variability in practices [11].
ESGE recommends the saline bleb injection method, in which normal saline is initially injected into the submucosa to verify the correct plane followed by injection of tattoo ink into the bleb [12, 13]. Recommendations continue to vary between many studies, including location of tattoo mark, number of tattoo marks, and injection technique [5, 8, 14-16] [1]. The ideal tattoo location is 3 cm or more distal to the lesion with placement of two to three separate marks on opposite sides of the lumen. This distance between lesion and tattoo injection avoids potential extension of tattoo beneath the lesion which carries the risk of submucosal fibrosis should endoscopic resection be desired, minimizes the risk of needle-track seeding, and importantly, conveys to the surgeon an appropriate oncologic distal resection margin. In our study, a minority of gastroenterologists (25.6%) but a majority of colorectal surgeons ( 76.7%) tattooed at the preferred distal location (p < 0>
Tattooing technique focuses on the deposition of ink into the submucosal space for optimal visualization of the mark from the peritoneal cavity or the colonic lumen. Introduction of the ink can be directed into the submucosa or via a two-step method with initial creation of a saline bleb in the submucosa followed by the injection of ink into the bleb [15]. The preferable technique for tattooing is injection of the dye upon advancement of the needle into the submucosal space, which likely limits inadequate transmural staining of tattoo as well as intra-peritoneal application [8]. Both specialties had a limited number of physicians using the preferred technique: 16.7% of gastroenterologists and 6.7% of colorectal surgeons (p= 0.227).
In our study, not all physicians (15 of 108, 14%) reported performing endoscopic tattooing for suspected malignant colonic lesions. We postulate that this could potentially be attributed to utilization of standard polypectomy, endoscopic mucosal resection or endoscopic submucosal dissection during the index colonoscopy. Another consideration is the common practice of not tattooing cecal or rectal lesions, as seen in the study conducted by Nahid et al [17]. The tattooing of lesions at certain locations such as cecum and rectum is controversial given that some physicians consider these locations to be dependable landmarks thus obviating the need for tattoo localization of lesion. However, as reported by Blum-Guzman et al [9] , relying solely on anatomy could lead to inaccurate localization. Tattooing of rectal lesions, exclusive of very distal lesions, is important as it allows for the precise demarcation of the distal margin and facilitates intraoperative transection at the desired margin, likely decreasing the risk of a positive distal resection margin [18, 19]. Incorrect tattooing could potentially lead to inaccurate surgical management [13, 17] [20]. For example, if both a distal and proximal tattoo were applied, however, only the proximal tattoo was apparent at time of surgery, the surgeon would typically assume this represented the distal margin and perform an inadequate operation. In addition, rectal cancers often receive neoadjuvant therapies with expected tumor regression. Occasionally, a rectal cancer may downsize and subsequently be difficult to identify intra-luminally, making tattoo placement at diagnosis critical. Less than half of the gastroenterologists (41%) tattooed rectal tumors, of which the response was mixed in regard to location compared to the majority of surgeons (87%) who reported tattooing distal to the rectal lesion (p=0.001). The remainder likely reflect very distal rectal lesions not amenable to sphincter-preserving operations, such that a tattoo would not be informative of a resection margin and would be unnecessary.
The number of tattoo marks placed to designate a certain lesion range from one to over four in our survey, though the majority of physicians report placing two to three marks. This is in accordance with ESGE recommendations, as this avoids the poor visibility of only one mark and decreases the likelihood of missing the marker intraoperatively. Specific to rectal lesions, the tattoo may be difficult to identify intraoperatively when injected only posteriorly into the mesorectum. In this specific anatomic scenario, the rectal wall is not visible during a total mesorectal excision, and emphasizes the importance of placing multiple marks around the circumference of the colorectum.
Our survey has demonstrated great variability in endoscopic tattooing practices between gastroenterologists and colorectal surgeons, and even within these respective groups. This known variability makes it very pivotal for detailed, accurate documentation of tattooing in the endoscopy report to facilitate the transmission of essential information between the endoscopist and surgeon. Our survey showed high compliance with documentation regarding the presence of and location of tattoos, but less so the number of tattoos; however, as established in Spaete et al [16], self-reported compliance with documentation can be overestimated when compared to rates of documentation on review of endoscopy reports.
Despite its statistically significant results, our study does has its limitations. First and foremost, this is a survey analysis with a small participant pool. Without the knowledge of how physicians and trainees were invited to participate in the survey, the impact of a response bias cannot be determined. Secondly, most of the participants were from academic institutions, which may not reflect the tattoo practices in its entirety, especially in the community setting. Third, is the unequal sample size between gastroenterologists and colorectal surgeons with a lower response rate among colorectal surgeons. This in turn could contribute to the discrepancies seen in our study and the opinions may not be generalizable.
Conclusion:
In conclusion, our study sheds light on the wide variability among colorectal surgeons and gastroenterologists on endoscopic tattooing practices with a dire need to standardize these guidelines nationwide, to properly guide subsequent operative resections.
Acknowledgements:
We would like to thank Dr. Jason Klapman and Dr. Seth Felder for review of the manuscript. We would also like to thank Dr. Ambuj Kumar for statistical analysis and manuscript review.
Conflicts of Interest:
There is no conflict of interest for any of the authors.
References
-
Piscatelli N, Hyman N, and Osler T. Localizing colorectal cancer by colonoscopy. Arch Surg, 2005. 140(10): p. 932-5.
Publisher | Google Scholor -
Zerey M, Hawver LM, Awad Z, Stefanidis D, Richardson W, et. al. SAGES evidence-based guidelines for the laparoscopic resection ofcurable colon and rectal cancer. Surg Endosc, 2013. 27(1): p. 1- 10.
Publisher | Google Scholor -
Shinagawa T, Tanaka T, Nozawa H, Emoto S, Murono K, et. al. Comparison of the guidelines for colorectal cancer in Japan, the USA and Europe. Ann Gastroenterol Surg, 2018. 2(1): p. 6-12.
Publisher | Google Scholor -
Wang CL, Qu G, and Xu HW. The short- and long-term outcomes of laparoscopic versus open surgery for colorectal cancer: a meta- analysis. Int J Colorectal Dis, 2014. 29(3): p. 309-20.
Publisher | Google Scholor -
Letarte F, Webb M, Raval M, Karimuddin A, Brown CJ, et. al. Tattooing or not? A review of current practice and outcomes for laparoscopic colonic resection following endoscopy at a tertiary care centre. Can J Surg, 2017. 60(6): p. 394-398.
Publisher | Google Scholor -
Beretvas RI and Ponsky J. Endoscopic marking: an adjunct to laparoscopic gastrointestinal surgery. Surg Endosc, 2001. 15(10): p. 1202-3.
Publisher | Google Scholor -
Zafar A, Mustafa M, and Chapman M. Colorectal polyps: when should we tattoo? Surg Endosc, 2012. 26(11): p. 3264-6.
Publisher | Google Scholor -
Rex DK. The Appropriate Use and Techniques of Tattooing in the Colon. Gastroenterology & Hepatology, 2018. 14(5): p. 314-316.
Publisher | Google Scholor -
Blum-Guzman JP and S. Wanderley de Melo Jr. Location of colorectal cancer: colonoscopy versus surgery. Yield of colonoscopy in predicting actual location. Endosc Int Open, 2017. 5(7): p. E642- E645.
Publisher | Google Scholor -
Kethu SR, Banerjee S, Desilets D, Diehl DL., Farraye FA., et. al. Endoscopic tattooing. Gastrointestinal Endoscopy, 2010. 72(4): p. 681-685.
Publisher | Google Scholor -
Ponsky JL and King JF. Endoscopic marking of colonic lesions. Gastrointest Endosc, 1975. 22(1): p. 42-3.
Publisher | Google Scholor -
Ferlitsch M, Moss A, Hassan C, Chandari P, Dumonceau J, et. al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy, 2017. 49(3): p. 270-297.
Publisher | Google Scholor -
Hyman N and Waye JD. Endoscopic four quadrant tattoo for the identification of colonic lesions at surgery. Gastrointest Endosc, 1991. 37(1): p. 56-8.
Publisher | Google Scholor -
Sawaki A, Nakamura T, Suzuki T, Hara K, Kato T, et. al. A two- step method for marking polypectomy sites in the colon and rectum. Gastrointest Endosc, 2003. 57(6): p. 735-7.
Publisher | Google Scholor -
Spaete JP, Zheng J, Chow S, Burbridge R, Garman K. Inconsistencies in Colonic Tattooing Practice: Differences in Reported and Actual Practices at a Tertiary Medical Center. South Med J, 2019. 112(4): p. 222-227.
Publisher | Google Scholor -
Kirchoff DD, Hang JH, Cekic V, Baxter K, Kumar P, et. al. Endoscopic tattooing to mark distal margin for low anterior rectal and select sigmoid resections. Surg Innov, 2014. 21(4): p. 376-80.
Publisher | Google Scholor -
Cipe G, Cengiz MB., Idiz UO., Yardimci E, Malya U, et. al. The Effects of Preoperative Endoscopic Tattooing on Distal Surgical Margin and Ileostomy Rates in Laparoscopic Rectal Cancer Surgery: A Prospective Randomized Study. Surg Laparosc Endosc Percutan Tech, 2016. 26(4): p. 301-3.
Publisher | Google Scholor -
Wang R, Hongli Z, Dazhou L, Haitao L, Li Y, et. al. [Application of endoscopic tattooing with carbon nanoparticlet in the treatment for advanced colorectal cancer]. Zhonghua Wei Chang Wai Ke Za Zhi, 2020. 23(1): p. 56-64.
| Google Scholor
