Review Article
- Dr. S. RAVINDRA BABU M.PHARM., PHD* 1
PROFESSOR Mallareddy institute of pharmaceutical sciences, email: ravicology@gmail.com
*Corresponding Author: Dr. S. RAVINDRA BABU M.PHARM., PHD*
Citation: Dr. S. RAVINDRA BABU M.PHARM., PHD* Non-Pharmacological Approaches to OA Pain Management in Conjunction with NSAIDs Medical and Clinical Laboratory Reviews 1(1). DOI: 10.9567/ISSN.2024/WSJ.97
Copyright: © 2024, Dr. S. RAVINDRA BABU M.PHARM., PHD*, this is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 07, 2024 | Accepted: November 11, 2024 | Published: November 29, 2024
Abstract
It is a progressive, degenerative joint disease that includes an inflammatory component and results in the destruction of cartilage .Since there are no disease-modifying treatments, current guidelines concentrate on managing symptoms. The aim of this study was the combined effect of non-steroidal anti-inflammatory drugs (NSAIDs) along with physical therapy in treatment for knee osteoarthritis. We studied 46 KOA patients from the Department of Physical Medicine and Rehabilitation, Emergency Clinical County Hospital of Craiova, Romania that have recieved for at least two months combined treatment with Diclofenac (150 mg/day maximum 10 days/month as needed) together with an ambulant physical therapy program over a period covering all year . The results revealed statistically significant reductions in WOMAC pain score and VAS (p = 0.0142 to 0023) with corresponding greater improvements in KOS-ADL & OKS function scores ( p=0128 ±.0023). Higher VAS with cholesterol level was positively correlated (p=0.0092), but not significantly associated by t-test for triglyceride levels (CHOL: r = 1, p Patients were followed-up for 24 weeks after the intervention to determine if any of them needed surgery. In summary, the results of this research demonstrated that combined NSAID and physical therapy treatment could be a viable individualized approach in reducing pain, improving joint function among patients with KOA.
Keywords: self-medication; knee osteoarthritis; hip osteoarthritis; WOMAC
Introduction
Osteoarthritis (OA), previously referred to as osteoarthrosis, is the most prevalent chronic and degenerative joint disorder that primarily affects synovial joints. It results in chronic joint pain due to the sequenced degeneration and ultimate loss of articular cartilage, which is a tissue that covers bone ends within synovial joints. This degradation then triggers a series of structural and functional changes across the entire joint complex, not only involving migrating cartilage but also affecting the synovium (joint lining), menisci (cartilaginous pads), tendons or ligaments and subchondral bone OA is the most known and often occurring form of arthritis surpassing its prevalence than rheumatoid or other type of articular ailment .
OA continues to be a growing problem in part because an aging, global population and rising rates of obesity are rendering the pain syndrome more prevalent. Consequently, the OA burden has reached epidemic proportions and is without doubt a major public health problem. In many regards, the pathogenesis of OA and pain generation in involved joints are better understood in recent years .
The socioeconomic consequences of OA are significant. OA results in work disability for at least 20 million people and annual costs likely exceeding $100 billion that ultimately burden the health care system of the United States alone. Just as in Europe, me and OA are two of the five most costly healthcare-associated costs .
Numerous risk factors have been elucidated that acts as the trigger in OA pathogenesis. Some of these are potential points for intervention, while others are not. Non-modifiable factors which could increase the likelihood of developing osteoarthritis would include age, being female and having a genetic predisposition as well as history of joint trauma such as with sports injuries or fractures that may lead to subsequent joint instability or muscle laxity. Other modifiable factors include high body mass index, which indicates overweight or obesity, frequent joint stress (The higher prevalence of OA in women, as compared to men further implicate the necessity for sex as a risk factor .
Managing OA effectively requires an accurate diagnosis. An array of imaging. techniques is used for screening, diagnosing and monitoring the disease process Table 1 outlines their relative strengths and weaknesses Current imaging strategies are helpful to evaluate OA as it is, and conventional radiography remains an inexpensive simple-to-inigate diagnostic CA approch. It helps in seeing the bony alterations like osteophyte whatever states bone spurs, joint space narrowing and subchondral sclerosis (increased bone density under the cartilage) and last of all shows us about Subchondral cysts .
Ultrasound, images of muscles joints and other soft tissue structures which when used in ante partum phases enhances radiographs. Meniscal extrusion, tibiofemoral osteophytes and changes in the medial femoral cartilage can be demonstrated more accurately on MSUS compared to radiography , likewise bursitis.
MRI has long been the gold standard for OA evaluation based on its capacity to image whole joints as organs. MRI enables concomitant evaluation of changes in multiple tissues as well as pre-morphological alterations in the biochemistry of articular and periarticular tissues. MRI is useful for the evaluation of structures that are not readily visible on plain radiographs (for example, articular cartilage, menisci, ligaments and synovium) as well as some other structures . MR is considerably more expensive, however it provides information about a marked higher number of severe joint pathologies which frequently happen to be necessary for surgical planning.
Literature Review
Play Synopsis: NSAID and Physical Therapy Combination for Knee Osteoarthritis
Knee osteoarthritis (OA) is a common, disabling condition accompanied by progressive cartilage degeneration and inflammation that can adversely affect the quality of life for patients. In the absence of disease-modifying treatments, management is oriented towards symptomatic control and improved function . The present literature review aims to evaluate the current evidence of non-steroidal anti-inflammatory drugs (NSAIDs) and physiotherapy in the management of KOA.
Nonsteroidal anti-inflammatory drugs (NSAIDs) for Pharmacological Management of KOA:
KOA is primarily treated through NSIADs use because of its analgesic and anti-inflammation effects (Moon et al., 2014). They do this by inbibiting cyclooxygenase enzymes, which play an important role in prostaglandin synthesis (pain and inflammation). For example, (Moon et al., 2014) mentioned aceclofenac as a case of better safety and tolerance profile because this NSAID has higher COX-2 selectivity. Nevertheless, long-term NSAID exposure is linked with GI adverse events and thus should be meticulously monitored for an individual patient's risk factors .A recent RCT from a different group reported the need to observe for and treat possible opioid-related adverse effects using non-pharmacological strategies in combination with pain-killers.
Treatment Modalities:Treatment modalities for KOA include the following: Physical therapy interventions
One of the cornerstones in KOA management is physical therapy, which targets both muscle strength and joint mobility deficits . Strength training, manual therapy, aquatic therapy, and balance training are a few within the range of physical modalities that have effectiveness in improving PD symptoms . Make reference to the importance of quadriceps strengthening in KOA: prevention and rehabilitation, including neuromuscular electrical stimulation or mechanical vibration .Moreover, indicate the association between patients that adhere to exercise and achieve superior improvements in pain, physical function, and self-perceived effects. knee orthoses as an adjunct to other treatment options, claiming extra support and possible biomechanical offloading prompted by reduced weight-bearing forces on the knee joint.
NSAID + Physical Therapy Combined Approach:
Although NSAID are effective in managing symptoms of OAK as well is physical therapy, the combination has been postulated to be provide synergistic effects. By reducing pain and inflammation, NSAIDs can help patients engage more fully in physical therapies. Physical therapy, in turn can enhance joint function, strength and range of mathematical functions may well slay the work on obtaining sector NSAID use. Many studies have presented outcomes after combination treatment showing of pain reduction, functional improvement and improved quality of life. However, the optimal combination of NSAID and physical therapy interventions is unclear, as well as their long-term effects in this combined approach. It states that the more therapy and exercises present in your personal treatment plan for fibromyalgia.
Future Research Directions:
Areas for Future Research
Finding the best NSAID and physical therapy pairings for subgroups of different KOA patients.
Strategies for increasing patient adherence to pharmacological and non-pharmacological treatments
Exploring the benefits of NSAID and physical therapy post within rheumatoid arthritis disease progression for patient outcomes.
The present study aims to determine the cost effectiveness of this combined approach in relation to other treatment options.
Selection and Evaluation of Recipients
Patients were chosen and ordered based on American College of Rheumatology criteria for knee osteoarthritis. Patients were recruited from the Department of Physical Medicine and Rehabilitation, Emergency Clinical County Hospital Craiova between January 2021 to April 2024.
Inclusion criteria were:
- Age 18 years or older
- Documented KOA diagnosis
Grade 2 or more on Kellgren-Lawrence grade
- Pain lasting more than 3 months
Exclusion criteria were:
- Presence of other joint disease
- Autoimmune rheumatic disease
Recent joint trauma, surgery or infection
- Chronic organ failure
- Previous history of neoplastic disease in the past five years
Table 1. Baseline characteristics of patients.
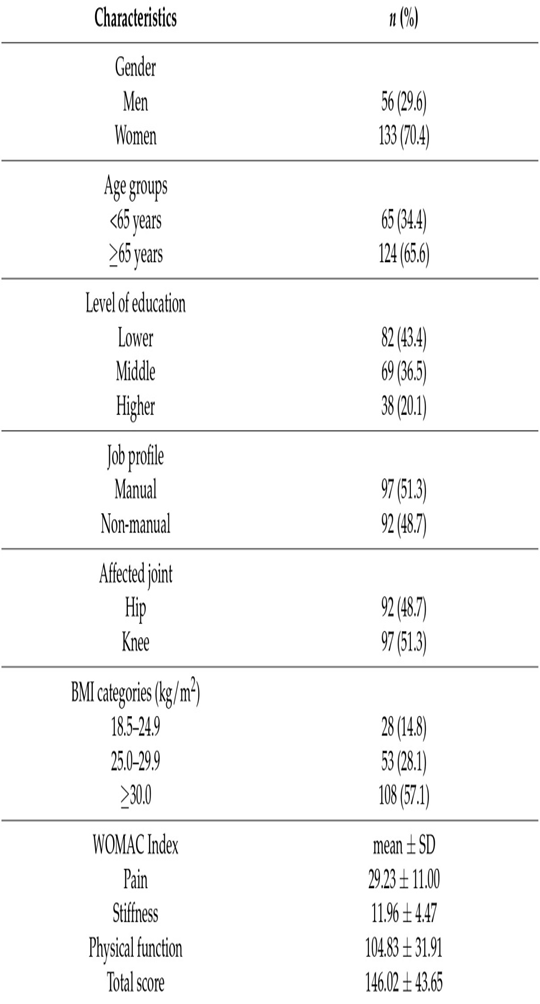
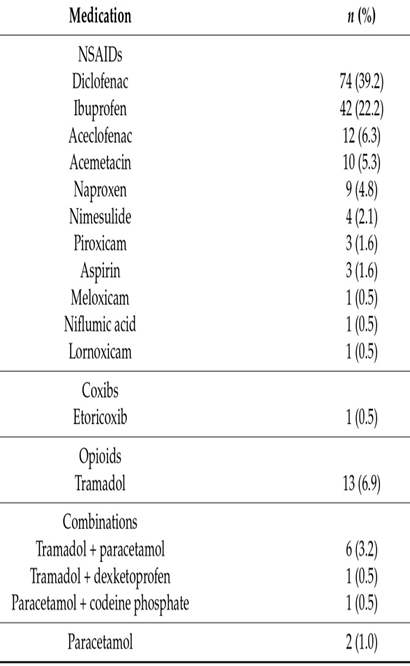
Table 2. Active ingredients of oral medications
Patients considered for redilation were those who fulfilled the criteria of a complete work-up comprising:-
1.Medical History: personal and family medical history was noted.
2 Physical Examination: Full clinical physical examination was undertaken, which included detailed inspection, palpation of the knee joint and effusion testing with an evaluation for both passive and active range of motion. Function, ligament and meniscus status were also evaluated.
3.Laboratory tests: They performed blood test.
4.Radiographic Study Anteroposterior (AP) and lateral radiographs of the knees were obtained for all patients. In the instance of surgical candidates, magnetic resonance imaging (MRI) was performed on the symptomatic knee.
5.Studied by Histopathology: Tissue samples were obtained during procedures for ment.
Nutritional Status: Body mass index was also calculated in order to evaluate nutritional status.
Functional Outcomes: Knee function during regular activities was as-sed using the following validated instruments.
Knee Outcome Survey Activities of Daily Living (ADL): 14-item questionnaire assessing symptoms (6 items, scored from 5 [no difficulty] to 0) and function on a visual analog scale format with a total score range of possible totals from zero to seventy. Higher scores mean better outcomes; Higher scores indicate better outcomes.
○ Western Ontario and McMaster Universities Osteoarthritis Index : A 24-item questionnaire evaluating pain, stiffness, and physical functions within the past 48 hours. Scores ranged from 0 (no) to four (extreme), with one for each item.
Pain Assessment: The pain intensity was evaluated by a 100 mm Visual Analog Scale.
Image and Histopathological Analysis
Anteroposterior (AP) and lateral radiographs were evaluated for joint space, osteophytes formation, and subchondral sclerosis. We classified the severity of osteoarthritis using The Kellgren-Lawrence grading scale
Sequences of the magnetic resonance imaging (MRI) were performed for knee:
- Proton density–fat saturation sagittal
- Coronal PD-FS
- Axial PD-FS
- Sagittal T1-weighted
- Coronal T1-weighted
- Sagittal T2-weighted
EVALUTION OF THE ANTERIOR CRUCIATE LIGAMENT SAGITTAL OBLIQUE PD-FS 27
Histological processing of tissue samples Tissue fragments from patients undergoing total knee replacement or arthroscopy were collected and processed to provide histopathology sections according to standard procedures defined in the literature . Briefly, 0.3 cm sections (perpendicular to the cartilage surface) were fixed in formalin for one to two days and decalcified extensively using EDTA before processing as above. Tissue processing for paraffin embedding was done on a Leica TP20 automatic tissue processor with 3-5 μm thick sections made using a semi-automatic microtome RM2255 from Leica. Sections were stained with Hematoxylin-Eosin (HE) and Safranin O targeting cartilage, respectively. Cartilage integrity and glycosaminoglycan content were evaluated using Safranin O staining (cartilage in orange, nuclei black).
Histopathological alterations were measured through Safranin O and HE staining. The loss of glycosaminoglycans is shown by the intensity of Safranin O staining [citation needed]. The nucleus was taken to home the ideal number of MSCs or MPCs based on cellularity and once this count reached a threshold, it would replicate resulting in natural division that drive corresponding enlargement (hypertrophy) rather than wear out; thus there exists very little proof since well before Safranin-O only labels dead metabolically dead cell matrix staining which could have promoted tidemark disruption . The OARSI grading system was used in order to describe the cartilage structure as follows: grade 0 – intact surface, grade 6 deformation (intermediate grades showed increasing levels of more severe damage including initial surface discontinuity; fissures and erosion).
Discussion
Objectives of the Study and Scope
The authors conducted a study to assess the combined benefits of oral nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy in terms of reduction in knee pain and improvement in functional performance among patients with knee osteoarthritis. The study notes that there are limitations, including its small sample size particularly when considering subjective measurements of pain. The main issue with the study, however, is that it had no control group so we can't be sure how much of this change was due to Christian involvement as opposed to outside forces.
Clinical Context & Treatment Guidelines
Osteoarthritis occurs most commonly in the knee [citation needed]. Several guidelines, such as those from the American College of Rheumatology [30], Osteoarthritis Research Society International (OARSI) ,European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) ,and either clinical practice guideline or appropriate use criteria, among others by the AAOS have been developed to guide KOA management. These guidelines are conservative and recommend pharmacological/non-pharmacologic treatment as first-line treatments, with surgery only for those who do not adequately respond to these.
Medications for Osteoarthritis
Oral NSAIDS have long been recommended for analgesia in OA but are associated with significant systemic toxicity via cyclooxygenase enzymes present in multiple tissues . Tieppo Francio et al. Narrative review compared oral diclofenac sodium with topical NSAIDs and/additionally acetaminophen, glucosamine/chondroitin sulfate vs placebo to propose 1st-line pharmacological management comprises topicals in addition or not combined w/oral instead of just one. For people who are otherwise healthy, however, oral NSAIDs remain a safe and provide an inexpensive option.
In a meta-analysis including 192 trials, reported on the safety and effectiveness of NSAIDs compared with opioids and acetaminophen for knee but not hip OA. Etoricoxib 60 mg/day and diclofenac 150 mg/day were found to be the most effective oral NSAIDs for pain relief and global status improvement, respectively. The researchers also underscored the diagnostic conundrum posed by adverse event risks from long-term dosing in patients with comorbidities. Because of lower systemic exposure and dose, topical diclofenac (70–81 mg/day) was suggested as a first-line treatment for KOA.
Conclusion
The aim of this study was to assess the benefit and safety from combining NSAIDs with physical therapy for treating knee osteoarthritis. Results indicate that KOA patients receiving a one-year interventional period with the combined treatment of Diclofenac (150 mg/day, maximum 10 days/month as needed) and an outpatient physical therapy program at Physical Medicine and Rehabilitation Department from Emergency Clinical County Hospital of Craiova demonstrated statistically significant improvements in most primary outcome measures.
Particularly, there were prominent reductions in both the WOMAC pain score and VAS (p = 0.0142 to 0.0023). These improvements in pain perception were reflected by comparable enhancements in functional capacity as evidenced by changes of the KOS-ADL/OKS function score .More over, correlation analysis showed a significant positive relation between VAS and cholesterol (p = 0.0092) along with non-significant association of triglyceride levels to SH prevalence. We have also seen that all patients were progression free in the MRI at 24 ± weeks of follow-up when both therapy was used.
These findings imply NSAIDs combined with physical therapy as an alternative noninvasive practice for KOA. This dual approach to pain and functional deficits could improve patient quality of life as well help defer or eliminate the need for more invasive procedures. Such a personalized treatment regimen optimizes how treatments are delivered to address an individual patient's specific requirements and circumstances.
However, it is necessary to put this study in context. The sample size was relatively small and the study conducted is single-center, so these findings may have limited generalizability. These training and NSAID recommendations may improve KOA patient outcomes, although future research is required to confirm these results in larger more diverse populations as well explore the best combined use of NSAIDs with physical therapy interventions among various subgroups within HCP OA patients. The other key element is long-term follow-up studies to evaluate the effect of such combined treatment approach over time.
Our findings overcome these limitations and provide important support for the effectiveness of combining NSAIDs with physical therapy in KOA management. The combined approach may be a useful clinical tool for clinicians trying to treat their KOA patients in an individualized and comprehensive manner.
References
-
Bocciardi, R., Bordo, D., Duca, M D., Rocco, M D., & Ravazzolo, R. (2008, October 1). Mutational analysis of the ACVR1 gene in Italian patients affected with fibrodysplasia ossificans progressiva: confirmations and advancements. Springer Nature, 17(3), 311-318. https://doi.org/10.1038/ejhg.2008.178
Publisher | Google Scholor -
Fibrodysplasia Ossificans Progressiva: Practice Essentials, Pathophysiology, Epidemiology. (2022, May 13)
--> -
Gregson, C L., Hollingworth, P., Williams, B., Petrie, K A., Bullock, A N., Brown, M A., Tobias, J H., & Triffitt, J T. (2010, October 30). A novel ACVR1 mutation in the glycine/serine-rich domain found in the most benign case of a fibrodysplasia ossificans progressiva variant reported to date. Elsevier BV, 48(3), 654-658. https://doi.org/10.1016/j.bone.2010.10.164
Publisher | Google Scholor -
Petrie, K A., Lee, W., Bullock, A N., Pointon, J J., Smith, R., Russell, R., Brown, M A., Wordsworth, B P., & Triffitt, J T. (2009, March 30). Novel Mutations in ACVR1 Result in Atypical Features in Two Fibrodysplasia Ossificans Progressiva Patients. Public Library of Science, 4(3), e5005-e5005. https://doi.org/10.1371/journal.pone.0005005
Publisher | Google Scholor -
Shore, J H M X E M. (2018, April 26). Variable signaling activity by FOP ACVR1 mutations. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5866189/
Publisher | Google Scholor -
Toksoy, M C B K O U. (2019, February 12). A Case of Fibrodysplasia Ossificans Progressiva in a 5-year-old Boy with all Musculoskeletal Features and Review of the Literature. https://pubmed.ncbi.nlm.nih.gov/30740372
Publisher | Google Scholor -
Makutam, Viswakanth & Achanti, Sai & Doostan, Marjan. (2024). INTEGRATION OF ARTIFICIAL INTELLIGENCE IN ADAPTIVE TRIAL DESIGNS: ENHANCING EFFICIENCY AND PATIENT-CENTRIC OUTCOMES. International Journal of Advanced Research. 12. 205-215. 10.21474/IJAR01/19245.
Publisher | Google Scholor -
Varagani, Srinivasarao & Safwan, Mohammad & Makutam, Viswakanth & Moparthi, Swapna & Vaishnavi, Sri & Kondru, Sowjanya & Yadav, Ritu & Dhiraj, Kohale. (2024). A comparative study on assessment of safety and efficacy of Diclofenac, Naproxen and Etoricoxib in reducing pain in osteoarthritis patients -An observational study. 10. 31-38. 10.22192/ijcrms.2024.10.08.003.
--> -
Priya, Maroju & Makutam, Viswakanth & Mohmed, Shaikh & Javid, Adnan & Safwan, Mohammad & Ahamad, Tanwir & Sathya, Alapati & Guptha, Sai & Dhiraj, Kohale & Mathew, Anannya & Varagani, Srinivasarao. (2024). AN OVERVIEW ON CLINICAL DATA MANAGEMENT AND ROLE OF PHARM.D IN CLINICAL DATA MANAGEMENT. World Journal of Advanced Pharmaceutical and Medical Research. 10. 299.
Publisher | Google Scholor -
Makutam, Viswakanth & Sundar, D & Vijay, M & Saipriya, T & Rama, B & Rashmi, A & Rajkamal, Bigala & Parameshwar, P. (2020). PHARMACOEPIDEMOLOGICAL AND PHARMACOECONOMICAL STUDY OF ANALGESICS IN TERTIARY CARE HOSPITAL: RATIONAL USE. World Journal of Pharmaceutical Research. 9. 787-803. 10.20959/wjpr20209-18206.
--> -
Makutam, Viswakanth. (2018). REVIEW ARTICLE ON FIBRODYSPLASIA OSSIFICANS PROGRESSIVA. 7. 359. 10.20959/wjpps20186-11696.
Publisher | Google Scholor
