RESEARCH ARTICLE
1Department of intensive care medicine, Saint Paul’s hospital millennium medical college, Addis Ababa, Ethiopia.
*Corresponding Author: : Muluneh Kidane Tufa, Department of intensive care medicine, Saint Paul’s hospital millennium medical college, Addis Ababa, Ethiopia.
Citation: Leea Tekle, Menbeu Sultan, Solomon Yimer, Muluneh Kidane, Knowledge, Attitude and Practice of Endotracheal Tube Suctioning and Associated Factors among Intensive Care Unit Nurses in Selected Public Hospitals in Addis Ababa, Ethiopia, 2024, Community and Public Wellness Nursing, vol 1[1]. DOI: 10.9567/3064-7061/WSJ.111
Copyright: © 2024, Muluneh Kidane Tufa, this is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: November 21, 2024 | Accepted: November 25, 2024 | Published: December 05, 2024
Abstract
Background: Endotracheal suctioning involves inserting a catheter into the endotracheal tube to remove lung secretions using negative pressure, which helps prevent secretion buildup, maintain clear airways, optimize oxygenation, and ultimately save patients' lives. Intensive care unit nurses' proficiency with endotracheal suctioning has a direct impact on minimizing the afore mentioned issues, raising the standard of care and shortening intensive care unit stays.
Objectives: To asses knowledge, attitude, practice of endotracheal tube suctioning and associated factors among intensive care unit Nurses in Selected Public Hospitals in Addis Ababa, Ethiopia, 2024.
Method: An institutional-based cross sectional study was conducted from 28th March- 28th June, 2024 at Selected Public Hospitals in Addis Ababa. Simple random sampling technique was conducted to get hospitals that were considered in the study. Data was collected by professional nurses using structured questionnaire. Analysis done using epinfo version 7.1 and SPSS version 25 software. Descriptive analysis logistic regression was also conducted. Predictors with p-value of <0.25 for bivariable & <0.05 for multivariable were considered statistically significant, indicating a significant relationship with the outcome variable.
Result: Among 229 nurses working in ICUs across selected hospitals. Nearly half of the nurses (48.5%) had poor knowledge, 57.6% demonstrated poor practice, and 59.8% had negative attitude towards performing endotracheal suctioning. Findings reveal significant associations between age, education level, experience, with both knowledge and practice of endotracheal suctioning. Nurses aged 26-30 and those with a Master's degree demonstrated higher knowledge and practice levels. Lack of institutional guidelines and inadequate training were barriers.
Conclusion and recommendation: ICU experience, and guideline availability play crucial roles in knowledge and practice of endotracheal suctioning, while education and training are critical for shaping their attitudes. Addressing these factors through tailored interventions is essential to improve patient care and outcomes.
Keywords: endotracheal suction, intensive care unit, Ethiopia
Introduction
Endotracheal suctioning [ETS] involves inserting a catheter into the endotracheal tube to remove lung secretions using negative pressure, which helps prevent secretion buildup, maintain clear airways, optimize oxygenation, and ultimately save patients' lives [1]. The fundamental goals of
ETS are to maintain gaseous exchange and airway permeability, promote alveolar ventilation, supply enough oxygen, and avoid ventilator-associated pneumonia [2].
An open suctioning system [OSS] and a closed suctioning system [CSS] are the two ways suctioning can be done [3].
In the OSS, patients are disconnected from the ventilator and suctioned. However, in the CSS, patients are suctioned without disconnection from the ventilator, and oxygenated air flows from the ventilator even during suctioning with the maintenance of partial ventilation and positive end-expiratory pressure [4].
Micro-aspiration of secretions is a risk factor for ventilator-associated pneumonia, so it's critical to evaluate procedures for oral suctioning, dental hygiene, and endotracheal tube management [5]. One of the most popular treatments for patients with respiratory diseases is airway suctioning [6]. ETS keeps the lungs from becoming too secreted, maintaining airway patency, ensuring appropriate oxygenation, and ultimately preserving the lives of the patients [7]. By clearing the airways, this technique maintains their permeability and promotes appropriate gas exchange [7,8]. Acute respiratory distress, deterioration of arterial blood gas and oxygen saturation levels, visible secretions in the airway, and probable aspiration of upper airway or gastric secretions are the indicators of ETS [9]. In addition to this frequent coughing, the presence of rhonchi, oxygen desaturation, a change in vital signs dyspnea, restlessness, elevated peak inspiratory pressure, or high-pressure ventilator alarms are among the signs that suctioning is necessary [10].
Open suctioning can result in hypoxemia, which is thought to be a frequent adverse effect [11]. Despite of ETS being a necessary procedure to both children and adult patients, if the procedure is not performed with correct techniques, it can lead to serious complications, such as bleeding, infection, hypoxia, bronchoconstriction, atelectasis, increase in intra-cranial pressure, cardiac arrest and sudden death [12]. Additionally, it was linked to dangers and outcomes include increased tracheal mucosa lesions and infections [13].
It is imperative to follow proper airway suctioning procedures to reduce the risk of complications like discomfort, anxiety, or frightening sensations, increased mucus secretions if done too frequently, hypoxemia [a drop in oxygen saturation], mucus membrane irritation, airway trauma, infection, and elevated intracranial pressure in patients with head injuries [14]. Hence the aim of this study was to asses knowledge, Attitude, practice and associated factors of endotracheal tube suctioning among ICU Nurses in Selected Public Hospitals in Addis Ababa, Ethiopia, 2024.
Materials and Methods
Study Area
Addis Ababa is a city that is home to a total of 53 hospitals, comprising 13 public hospitals and 40 hospitals managed by NGOs and private organizations(37). Among the public hospitals, there are seven federal hospitals: Tikur Anbesa Specialized Hospital (TASH), St. Paul's Hospital Millennium Medical College (SPHMMC), Addis Ababa Burn, Emergency and Trauma (AaBET) which is affiliated with St. Paul's Hospital, St. Peter Hospital, Amanuel Hospital, Yeka Kotebe Hospital which is affiliated with Amanuel Hospital, and Alert Hospital. In addition to the federal hospitals, there are six hospitals administered by the Addis Ababa City Administration: Yekatit 12 Hospital, Minilik Hospital, Zewditu Hospital, Gandhi Hospital, Tirunesh Bejing Hospital, and Ras Desta Hospital.
There are around 396 nursing staffs working in ICU (both adult and pediatric ICU) nurses.
Study design and period
An institutional-based cross sectional study was conducted from 28th March – 28 June 2024, to assess knowledge, attitude and practice of endotracheal tube suctioning among ICU Nurses in Selected Public Hospitals in Addis Ababa, Ethiopia, 2024.
Source and study population
The source population for the study included all nurses working in both adult and pediatric ICUs of public hospitals in Addis Ababa. All nurses working in the six selected public hospitals ICUs during the data collection period that fulfilled the inclusion criteria.
Inclusion and exclusion criteria
Nurses who were working in ICU for 6 months and above in selected public hospitals in Addis Ababa as full time employees, those nurses who were available on the study time and were agreed to consent were considered in the study. All part-time nurses, nurses with less than 6 months of work experience, nurses who nurses who were not available during the study period were excluded from the study.
Sample size determination
Sample size for the study was determined by using single population proportion formula with considering P=28.9% (a study conducted in Amhara region public hospitals)(14), with the assumption of 95% confidence interval (CI), 4% margin of error, and 10% nonresponse rate.

n: sample size
Z: desired 95% confidence, Z=1.96(from normal distribution table).
P: Practice of endotracheal tube suctioning among ICU Nurses.
d: margin of error (0.04).

Adding a 10% ( ) for non-response rate, the total number sample estimated was
) for non-response rate, the total number sample estimated was
In addition, since the total number of nurses working in ICU are 396 which is less than 10,000, and if  > 0.05 correction formula was used. Then, 542/396
> 0.05 correction formula was used. Then, 542/396 which indicates need of correction for sample size calculation.
which indicates need of correction for sample size calculation.
 =nf
=nf
nf= corrected sample size
ni= sample size calculated early
N= total population in the study area
Substituting the values =542/ 2.365=229
Sampling technique and Procedure
To ensure a representative sample, the researcher first was employing a simple random sampling technique. Thirteen public hospitals in Addis Ababa were identified as the sampling frame. From this frame, six hospitals were selected using a lottery method, ensuring an unbiased selection process. The chosen hospitals were SPHMMC
AaBET, St. Peter, Yeka Kotebie, Zewditu and Tirunesh Bejing.
Considering the small number of ICU nurses in each hospital and the desire to include all eligible participants, the researcher decided to employ a census method. This means that instead of selecting a sample from the population, the researcher aims to include the entire population of ICU nurses from the selected hospitals.
Table 1: Schematic presentation of sampling procedure in public hospital in Addis Ababa, 2024.
| Hospitals | SPHMMC | AaBET | St. Peter | Yeka Kotebie | Zewditu | Tirunesh Bejing |
| Number of ICU nurses | 73 | 40 | 30 | 35 | 26 | 25 |
4.8 Study variables
- Dependent Variable
- Knowledge endotracheal tube suctioning
- Practice endotracheal tube suctioning
- Attitude endotracheal tube suctioning
- Independent Variables
- Socio-demographic characteristics:
- Age
- Sex
- Educational Status
- Marital Status
- Experience
- Attitude towards endotracheal tube suctioning
- Institutional related parameters
- Training
- Adequacy of equipment
- Availability of guideline
Data collection tools and procedure
The data was collected using a structured questionnaire that includes socio-demographic information as well as Knowledge, attitude and practice of endotracheal tube suctioning. The tool was created after studying relevant, similar literature reviewed and was written in English. Data collectors (three professional nurses) and supervisors (one public health professional) were hired to collect the data.
Data Quality Assurance
Before starting data collection from the participants, a thorough quality check of the data collection tool was performed. This involved conducting a 5% pretest prior to the actual study. The data collectors and supervisors received a one-day training session, and a pretest was conducted to assess the appropriateness and effectiveness of the questionnaire.
To ensure data integrity, the investigator closely monitored the data collection process and reviewed the collected data for completeness, correctness, and consistency. This step was taken before leaving the actual data collection site.
Data processing and analysis
Throughout the data collection process, the consistency and completeness of the data was reviewed. Each questionnaire was given a code with a unique identification for each questioner, which was then entered into Epinfo version 7.1 then analyzed using SPSS software version 25. Running frequencies and cross tabulation data was used to check for missing values and outliers. Each independent variable was cross tabulated using bivariate analysis for the dependent variable Knowledge, practice and attitude of endotracheal tube suctioning. Binary logistic regression was used to examine the association between each independent variable and Knowledge, practice and attitude of endotracheal tube suctioning.
To rule out cofounding variables, binary logistic regression analysis was performed using of each independent variables with the dependent variable. The adjusted odds ratio (AOR) and 95 percent confidence interval (CI) was used as indicators to measure the strength, direction, and significance of the association. Factors having a bivariable logistic regression p-value of less than 0.25 was fitted into multivariable logistic regression, then those having a p-value of <0>
Ethical Consideration
The Saint Paul’s Hospital Millennium Medical College review board (IRB) will approve the study, and a support letter was obtain from each hospitals. After describing the study's goal, each participant was given their consent. Participants' right to identity and confidentiality was respected. The volunteers was not harmed in any way during the study.
Result
Socio-Demographic Characteristics
This study was conducted among 229 nurses currently working in ICU across selected hospitals in Addis Ababa, achieving a response rate of 100%. Among these nurses, the majority (77.7%) are aged between 26-30 years. A smaller percentage are under 25 years (3.5%), while 14.0?ll in the 31-35 age range, and 4.8% are older than 36. Regarding the sex of study participants, the majority (57.6%) were male.
In terms of educational attainment, 81.2% of the participants hold a Bachelor's degree (BSc), while 18.8% possess a Master's degree (MSc). Regarding marital status, a majority of the nurses are single (60.3%), followed by those who are married (38.9%). Only a small fraction of participants reported being separated (0.9%).
Professionally, a significant portion of the nurses (38.0%) had 6-10years prior work experience as nurses before their current roles in ICU. Among those with ICU experience, the majority (80.8%) have worked in ICU for less than 5 years, while 18.8% have 6-10 years of ICU experience.
Table 2: Socio-demographic characteristics of nurses working in Adult & Pediatric intensive care units in Addis Ababa, 2024 (n=229).
Institutional Related Characteristics
This finding revealed that 34.1% of the nurses have received training relevant to their roles in ICU, whereas the remaining 65.9% have not received such training. The availability of equipment in ICU settings is high, with 90.0% of participants reporting access to necessary equipment. However, guidelines are less universally accessible, with only 22.3% of nurses indicating that guidelines are readily available in their workplace. Regarding the specific ICU units where nurses work, a significant majority (76.9%) are working in Adult Intensive Care Units, while the remaining 23.1% of the study participants are working in Pediatric Intensive Care Unit.
Table 3:Institutional related characteristics of nurses working in Adult & Pediatric ICU, Addis Ababa, Ethiopia, 2024 (n=229)
| Variable | Response | Frequency | Percent |
| received training | No | 151 | 65.9 |
| Yes | 78 | 34.1 | |
| equipment | No | 23 | 10.0 |
| Yes | 206 | 90.0 | |
| availability of guideline | No | 178 | 77.7 |
| Yes | 51 | 22.3 | |
| working unit | AICU | 176 | 76.9 |
| PICU | 53 | 23.1 |
Knowledge of nurses towards suctioning endotracheal suctioning
The majority (62.4%) agree that suctioning should only be performed based on a thorough patient assessment rather than routine, emphasizing a patient-centered approach to care that considers individual needs and conditions. Regarding patient participation in secretion management, an overwhelming majority (94.3%) advocate for encouraging patients who are capable of coughing up their own secretions to do so. In terms of technical considerations, most respondents (92.6%) agree that suction catheters should be appropriately sized—small enough to minimize discomfort and trauma, yet large enough to effectively remove secretions. Similarly, a majority (92.6%) believe that the suction catheter should not occlude more than half of the artificial airway's internal diameter to prevent excessive negative pressures and potential oxygenation issues.
Regarding suction system preferences, a significant majority (77.3%) endorse the use of a closed suction system for adult patients with specific respiratory considerations such as high oxygen concentrations or positive end-expiratory pressure (PEEP), aligning with guidelines aimed at reducing infection risks and maintaining respiratory stability. There is also a notable consensus (66.4%) that neither closed nor open suction systems hold superiority over the other in various aspects including oxygen saturation, cardiovascular stability, secretion removal efficiency, environmental contamination, and cost-effectiveness.
In terms of procedural techniques, opinions vary on the use of normal saline instillation before suctioning, with a slight majority (52.8%) suggesting its routine use should be avoided, highlighting ongoing debate and varying practices regarding its efficacy and potential complications. Furthermore, a strong majority (96.5%) agree that ensuring adequate patient hydration facilitates the removal of respiratory secretions.
Technical nuances such as the depth of suction catheter insertion and the use of hyperinflation techniques are also considered important by respondents, with significant majorities supporting specific practices aimed at optimizing suctioning efficacy while minimizing potential complications such as hypoxemia and cardiovascular instability.
Table 4: Distribution of knowledge score among nurses working in Adult & Pediatric ICU towards suctioning artificial airway, 2024 (n=229).
| Statement | Response | Frequency |
| Suctioning should only be done when a thorough assessment of the patient establishes the need for such a procedure and not be dictated by routine | No | 86 (37.6) |
| Yes | 143(62.4) | |
| If patients are able to cough up their own secretions, they should be encouraged to do so | No | 13(5.7) |
| Yes | 216(94.3) | |
| Suction catheters should be as small as possible, yet large enough to facilitate secretion removal | No | 17(7.4) |
| Yes | 212(92.6) | |
| The size of the suction catheter should occlude no more than half of the internal diameter of the artificial airway to avoid greater negative pressures in the airway and to potentially minimize falls in PaO2 | No | 17(7.4) |
| Yes | 212(92.6) | |
| The use of a closed suction system is suggested for adults with high FIO2 or PEEP, or at risk for acute lung injury | No | 52(22.7) |
| Yes | 177(77.3) | |
| The closed or open suction system is not superior to the other in terms of oxygen saturation, cardiovascular instability, secretion removal, environmental contamination, and cost | No | 77(33.6) |
| Yes | 152(66.4) | |
| Routine use of normal saline instillation prior to endotracheal suction should not be performed | No | 108(47.2) |
| Yes | 121(52.8) | |
| Ensuring patients are adequately hydrated is the way health care providers can facilitate the removal of respiratory secretions | No | 8(3.5) |
| Yes | 221(96.5) | |
| The suction catheter should be inserted to the carina and then retracted 1–2 cm before suctioning is performed, or the length of the suction catheter is estimated by measuring an identical endotracheal tube | No | 28(12.2) |
| Deep suctioning is necessary for patients with large amounts of secretions in the lower airways | Yes | 201(87.8) |
| Using volumes of hyperinflation that is indexed to the size of the patient may assist in minimizing potential difficulties | No | 43(18.8) |
| Yes | 186 (81.2) | |
| Tidal volumes should no more than 900 cc during hyperinflation because patients may feel dyspneic | No | 36(15.7) |
| Yes | 193(84.3) | |
| If hyperinflation is used in the patients before suctioning, caution should be employed because it may be associated with increases in mean arterial blood pressure | No | 17(7.4) |
| Yes | 212(92.6) | |
| Pre-oxygenation by the delivery of 100 % oxygen for at least 30 s prior to and after the suctioning procedure is recommended to prevent a decrease in oxygen saturation, especially when the patient has a clinically important reduction in oxygen saturation with suctioning | No | 49(21.4) |
| Yes | 180(78.6) | |
| Combining hyper oxygenation and hyperinflation prior to suctioning can minimize suctioning-induced hypoxemia | No | 23(10) |
| Yes | 206(90) | |
| A ventilator should be used rather than a manual resuscitation bag to provide hyperventilation/ hyper oxygenation prior to suctioning to reduce hemodynamic alterations | No | 20(8.7) |
| Yes | 209(91.3) | |
| Endotracheal suctioning, unless managed appropriately, can lead to various adverse events | No | 25(10.9) |
| Yes | 204(89.1) |
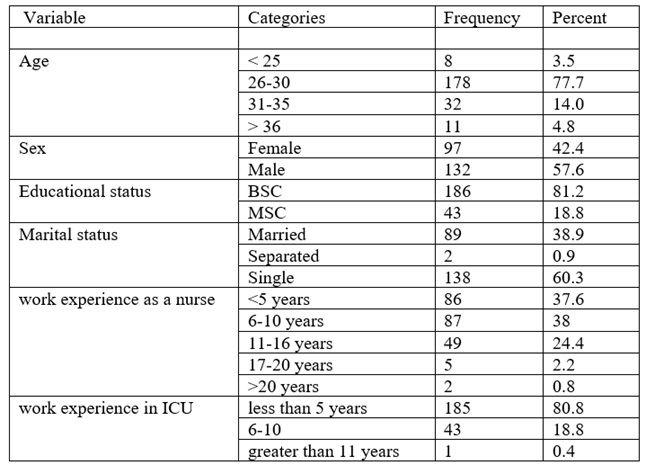
As illustrated in figure 2, nearly half of the nurses, comprising 48.5%, are categorized as having poor knowledge. Conversely, remaining nurses, 51.5%, are classified as possessing good knowledge.
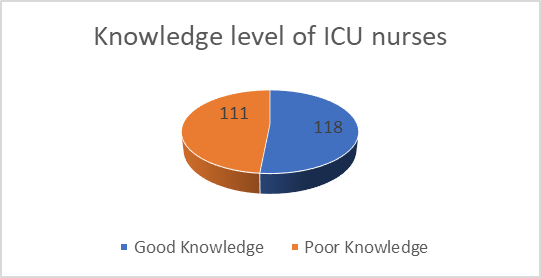
Figure 2:Over all knowledge score among nurses working in Adult & Pediatric ICU towards suctioning, 2024 (n=229).
Practice of ICU nurses towards endotracheal suctioning
Before initiating suctioning, nearly all nurses (96.9%) prioritize patient safety by diligently monitoring vital signs, including blood pressure, temperature, pulse rate, and oxygen saturation. Additionally, a majority (95.6%) ensure that the indication for suctioning is clearly identified, demonstrating clinical judgment in determining the necessity of intervention based on patient-specific needs. Moreover, all nurses (100%) consistently prepare essential equipment, ensuring readiness to perform the procedure efficiently and effectively.
During the suctioning process, ICU nurses adhere to established protocols aimed at optimizing patient comfort and procedural efficacy. While a significant majority (68.6%) position patients in semi-Fowler's position to facilitate airway management and patient comfort, fewer nurses (57.6%) routinely auscultate breath sounds to monitor lung status during suctioning. However, the use of a sterile towel on the patient's chest is less commonly practiced (21.8%).
Technically, ICU nurses demonstrate proficiency in employing sterile techniques and procedural guidelines to minimize risks and maximize patient safety. A substantial majority (73.8%) prioritize maintaining sterility when detaching suction catheter circuits, crucial for preventing infection and ensuring procedural integrity. Similarly, most nurses (79%) carefully insert suction catheters using gentle techniques, minimizing patient discomfort and reducing the likelihood of complications. During catheter withdrawal, a significant majority (71.2%) rotate the catheter 360 degrees, enhancing secretion removal efficiency and maintaining airway patency. Nurses also adhere to recommended suctioning times (71.2%), limiting suction duration to 10-15 seconds to balance effective secretion removal with patient comfort and safety.
All nurses (100%) consistently reassess vital signs post-suctioning, ensuring immediate evaluation of any procedural impact on patient stability and respiratory function. A strong majority (94.3%) adhere to guidelines that prohibit reinserting suction catheters into endotracheal tubes after use, mitigating the risk of contamination and potential respiratory complications. Furthermore, a majority (85.2%) maintain infection control practices by washing hands promptly after completing the suctioning procedure, essential for preventing cross-contamination and maintaining overall hygiene standards in ICU environments.
In documentation and disposal practices, nurses ensure comprehensive record-keeping by documenting secretion characteristics and ventilator settings (91.3%) post-suctioning. However, there is variability in immediate disposal of used supplies (26.6%), suggesting opportunities for standardizing post-procedural cleanup practices across healthcare settings.
Table 5:Distribution of practice score among nurses working in Adult & Pediatric ICU towards suctioning artificial airway, 2024 (n=229).
| Statement | Response | Frequency |
| Prior suctioning | ||
| Monitor vital sign (BP, temperature, PR, oxygen saturation) | No | 7 (3.1) |
| Yes | 222(96.9) | |
| Identify indication of suctioning | No | 10(4.4) |
| Yes | 219(95.6) | |
| Prepare equipment | Yes | 229(100) |
| Auscultate breath sounds | No | 97(42.4) |
| Yes | 132 (57.6) | |
| Check functionality of suction apparatus | No | 3(1.3) |
| Yes | 226(98.7) | |
| Check suction machine with connecting tube | No | 5 (2.2) |
| Yes | 224(97.8) | |
| Check availability of sterile normal saline | No | 10(4.4) |
| Yes | 219(95.6) | |
| Prepare ambu bag with oxygen supplies | No | 11(4.8) |
| Yes | 218 (95.2) | |
| Make sure that suction pressure at 80-120 mmHg | No | 82(35.8) |
| Yes | 147 (64.2) | |
| Wash hand | No | 70(30.6) |
| Yes | 159 (69.4) | |
| Wear mask | No | 29 (12.7) |
| Yes | 200 (87 3) | |
| Pre oxygenate the patient | No | 8 (3.5) |
| Yes | 221(96.5) | |
| During suctioning | ||
| Explain procedure to patient | No | 88 (38.4) |
| Yes | 141(61.6) | |
| Position patient in semi fowlers position | No | 72 (31.4) |
| Yes | 157 (68.6) | |
| Place sterile towel on patients chest | No | 179 (78.2) |
| Yes | 50(21.8) | |
| Open sterile glove | No | 96 (41.9) |
| Yes | 133 (58.1) | |
| Open sterile gloves, designate one hand(non-dominant) as clean | No | 165 (72.1) |
| Yes | 64(27.9) | |
| Use sterile hand to remove the suction catheter | No | 117 (51.1) |
| Yes | 112 (48.9) | |
| Detach circuit and maintain sterility | No | 60 (26.2) |
| Yes | 169 (73.8) | |
| Gently but quickly insert artificial airway using sterile technique | No | 48 (21) |
| Yes | 181(79) | |
| Don’t apply suction while inserting | No | 55(24) |
| Yes | 174(76) | |
| 360 rotation when withdrawing the catheter | No | 66 (28.8) |
| Yes | 163(71.2) | |
| Suctioning time 10-15 second | No | 66 (28.8) |
| Yes | 163 (71.2) | |
| Discontinue if HR is below or above normal | No | 20 (8.7) |
| Yes | 209 (91.3) | |
| Return patient to the ventilator | No | 12 (5.2) |
| Yes | 217(94.8) | |
| Rinse the catheter and connecting tube with normal saline | No | 3 (1.3) |
| Yes | 226 (98.7) | |
| Assess for secretion clearance | No | 10 (4.4) |
| Yes | 219 (95.6) | |
| Don’t perform more than 4 suction per suctioning | No | 8 (3.5) |
| Yes | 221 (96.5) | |
| Don’t reinsert suction catheter into endotracheal tube once used | No | 52 (22.7) |
| Yes | 177 (77.3) | |
Assess patients’ cardiopulmonary status
| No | 160 (69.9) |
| Yes | 69 (30.1) | |
| Post suctioning | ||
| Hyper oxygenate after suctioning | No | 13( 5,7) |
| Yes | 216(94.3) | |
| Return suction device | No | 65(28.4) |
| Yes | 164(71,6) | |
| Reassess patient vital signs | No | 6(2.6) |
| Yes | 223(97.4) | |
| Discard used supplies | No | 168(73.4) |
| Yes | 61(26.6) | |
| Wash hands | No | 34(14.8) |
| Yes | 195(85.2) | |
| Document type, amount, color of secretion and ventilator settings | No | 20(8.7) |
| Yes | 209(91.3) | |
As illustrated in figure 3, 57.6% of nurses working in the ICU showed poor practice, whereas 42.4% of the ICU nurses were demonstrated good practice

Figure 3:Over all practice score among nurses working in Adult & Pediatric ICU towards suctioning, 2024 (n=229).
Attitude of nurses towards endotracheal suctioning
A significant majority of ICU nurses (68.1%) strongly agree that assessing the patient to identify the need for suctioning is essential. However, despite recognizing the importance of patient assessment, a notable portion (65%) also acknowledges that suctioning is time-consuming. Regarding the necessity of suctioning, opinions are divided, with a substantial majority (52.4%) disagreeing that all ICU patients require suctioning upon admission.
When considering the clinical outcomes associated with suctioning, there is strong agreement (61.1%) that sterile suctioning can prevent ventilator-associated pneumonia (VAP). Furthermore, the responsibility for suctioning is widely recognized among ICU nurses, with a majority (60.2%) agreeing that it falls within their professional duties. In terms of procedural effectiveness, a majority (57.2%) disagree with the notion that suctioning is ineffective for thick and sticky secretions.
Additionally, there is strong support (73%) for the appropriateness of using suctioning to manage excessive secretions, highlighting its integral role in addressing respiratory complications commonly observed in critically ill patients. Hygiene practices related to suctioning also emerge as a significant consideration, with a majority (70.3%) agreeing on the importance of cleaning suction catheters with saline post-procedure.
As illustrated in figure below, 59.8% of the ICU nurses working in the hospital possessed a negative attitude, while 40.2% displayed a positive attitude.
Table 6. Attitude of nurses working in Adult & Pediatric ICU towards ETS, 2024 (n=229)
| Statement | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
Nurses should assess the patient to identify the need to suction | 2(0.9) | 0 | 4(1.7) | 67(29.3) | 156(68.1) |
| Suctioning is time consuming | 65(28.4) | 84(36.7) | 13(5.7) | 36(15.7) | 31(13.5) |
All patients who are admitted in the ICU need suctioning | 22(9.6) | 120(52.4) | 24(10.5) | 52(22.7) | 11(4.8) |
Give priority of care for patients with accumulated secretions | 3(1.3) | 1(0.4) | 13(5.7) | 102(44.5) | 110(48) |
| VAP* can be prevented by sterile suctioning | 3(1.3) | 0 | 76(4.4) | 140(33.2) | 229(61.1) |
| Suctioning is nurse’s responsibility | 17(7.4) | 0 | 45(12.7) | 69(30.1) | 69(30.1) |
Suctioning is ineffective for thick and sticky secretions | 43(18.8) | 88(38.4) | 50(21.8) | 34(14.8) | 14(6.1) |
Suctioning isn’t appropriate method for excessive secretions | 67(29.3) | 100(43.7) | 23(10) | 25(10.9) | 14(6.1) |
No need to clean suction catheter with saline after procedure | 78(34.1) | 83(36.2) | 13(5.7) | 42(18.3) | 13(5.7) |
Risk of VAP* can be decreased by sterile suctioning | 4(1.7) | 5(2.2) | 14(6.1) | 80(34.9) | 126(55) |
Suctioning prevents secretions to contaminate patient, nurse & environment | 2(0.9) | 22(9.6) | 12(5.2) | 120(52.40 | 73(31.9) |
Nurses spend less time while suctioning procedure | 12(5.2) | 55(24) | 57(24.9) | 85(37.1) | 20(8.7) |
Suctioning prevents hypoxemia, atelectasis and cardiac arrhythmia | 3(1.3) | 7(3.1) | 23(10) | 122(53.3) | 74(32.3) |
Suction catheter increases risk of bleeding complication | 9(3.9) | 19(8.3) | 37(16.2) | 144(62.9) | 20(8.7) |
| Statement | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree |
Nurses should assess the patient to identify the need to suction | 2(0.9) | 0 | 4(1.7) | 67(29.3) | 156(68.1) |
| Suctioning is time consuming | 65(28.4) | 84(36.7) | 13(5.7) | 36(15.7) | 31(13.5) |
All patients who are admitted in the ICU need suctioning | 22(9.6) | 120(52.4) | 24(10.5) | 52(22.7) | 11(4.8) |
Give priority of care for patients with accumulated secretions | 3(1.3) | 1(0.4) | 13(5.7) | 102(44.5) | 110(48) |
| VAP* can be prevented by sterile suctioning | 3(1.3) | 0 | 76(4.4) | 140(33.2) | 229(61.1) |
| Suctioning is nurse’s responsibility | 17(7.4) | 0 | 45(12.7) | 69(30.1) | 69(30.1) |
Suctioning is ineffective for thick and sticky secretions | 43(18.8) | 88(38.4) | 50(21.8) | 34(14.8) | 14(6.1) |
Suctioning isn’t appropriate method for excessive secretions | 67(29.3) | 100(43.7) | 23(10) | 25(10.9) | 14(6.1) |
No need to clean suction catheter with saline after procedure | 78(34.1) | 83(36.2) | 13(5.7) | 42(18.3) | 13(5.7) |
Risk of VAP* can be decreased by sterile suctioning | 4(1.7) | 5(2.2) | 14(6.1) | 80(34.9) | 126(55) |
Suctioning prevents secretions to contaminate patient, nurse & environment | 2(0.9) | 22(9.6) | 12(5.2) | 120(52.40 | 73(31.9) |
Nurses spend less time while suctioning procedure | 12(5.2) | 55(24) | 57(24.9) | 85(37.1) | 20(8.7) |
Suctioning prevents hypoxemia, atelectasis and cardiac arrhythmia | 3(1.3) | 7(3.1) | 23(10) | 122(53.3) | 74(32.3) |
Suction catheter increases risk of bleeding complication | 9(3.9) | 19(8.3) | 37(16.2) | 144(62.9) | 20(8.7) |
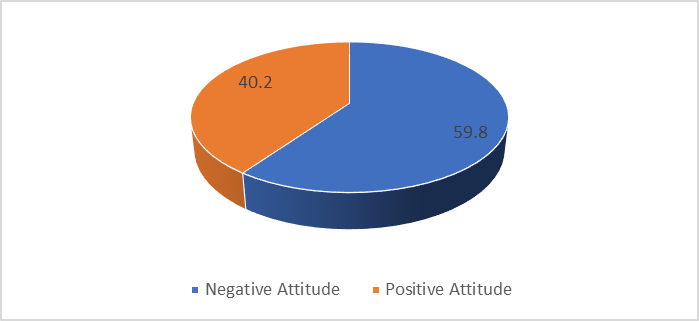
Figure 4: Over all Attitude score among nurses working in Adult & Pediatric ICU towards suctioning, 2024 (n=229).
Factors associated with knowledge towards endotracheal suctioning
In this study, few variables, such as age, availability of equipment, work experience and availability of guidelines variables were selected for multivariable analysis using binary logistic regression with a p-value less than 0.25. In the final multivariable logistic regression analysis, age in years and work experience of nurses working in ICU were linked with knowledge of endotracheal suctioning, as show in the table 7
Intensive care nurses with age range of 26-30 years are 5 time more likely have good knowledge compared to those ICU nurse with greater than 36 years of age [AOR=4.9; 95%CI: 1.8, 23.4]. Similarly, ICU nurses those who had work experience less than five years were 64% less likely to have good knowledge about endotracheal suctioning compared those who had work experience 6-11 years [AOR=0.36; 95%CI: 0.154, 0.82].
Table 7: Factors associated with level of knowledge among nurses working in ICU, Addis Ababa, Ethiopia (n=229)
| Variables | categories | Knowledge | P-value | COR | P-Value | AOR | |
| Good | Poor | ||||||
| Age | < 25> | 1 | 7 | 0.739 | 0.64(0.048,8.618) | 0.639 | 0.52(0.035,7.832) |
| 26-30 | 97 | 81 | 0.034 | 5.4(1.132,25,653) | 0.049** | 4.9(1.8 ,23.4) | |
| 31-35 | 18 | 14 | 0.041 | 5.8(1.074,31.163) | 0.063 | 5(0.92,27.65} | |
| >36 | 2 | 9 | 1 | 1 | 1 | 1 | |
| Experience in ICU | <5> | 94 | 101 | 0.019 | 0.39(0.176,0.854) | 0.016** | 0.36(0.154,0.82) |
| 5-11 | 24 | 10 | 1 | 1 | 1 | 1 | |
| Equipment | No | 7 | 16 | 0.038 | 0.37(0.148,0.95) | 0.066 | 0.4(0.151,1.061) |
| Yes | 111 | 95 | 1 | 1 | 1 | 1 | |
| Guideline | No | 96 | 82 | 0.175 | 1.54(0'824,2.891)2 | 0.202 | 1.55(0.79,3.048) |
| Yes | 22 | 29 | 1 | 1 | 1 | 1 | |
Factors associated with practice of endotracheal suctioning
In this study, four variables, such as age, educational level, availability of equipment and availability of guidelines variables were selected for multivariable analysis using binary logistic regression with a p-value less than 0.25. In the final multivariable logistic regression analysis, age availability of guideline and educational status in ICU were linked with knowledge of endotracheal suctioning, as show in the table 8
Intensive care nurses under the age of 25 were 97% less likely to perform endotracheal suctioning compared to those over 36 years old [AOR=0.03; 95%CI: 0.002, 0.05].. Likewise, ICU nurses aged 26-30 were 88% less likely to engage in this practice compared to their counterparts over 36 years of age [AOR=0.12; 95%CI: 0.023, 0.623].
Among nurses working in the ICU, those with a Master of Science degree were twice as likely to perform endotracheal suctioning compared to those with a Bachelor of Science degree [AOR=2.35; 95%CI: 1.065, 5.179]. Nurses working in ICU where guidelines were not available were 60% less likely to perform endotracheal suctioning compared to those in units with guidelines [AOR=0.4; 95%CI: 0.19, 0.75].
Table 8: Factors associated with level of Practice of among nurses working in ICU, Addis Ababa, Ethiopia (n=229)
| Variable | Categories | Practice | P-Value | COR | P-Value | AOR | |
| Good | Poor | ||||||
| Age | <25> | 1 | 7 | 0.009 | 0.032(0.002,0.426) | 0.010** | 0.03(0.002,0.5) |
| 26-30 | 68 | 110 | 0.013 | 0.14(0.029,0.66) | 0.012** | 0.12(0.23,0.623) | |
| 31-35 | 19 | 13 | 0.191 | 0.32(0.06,1.755) | 0.226 | 0.34(0.06,1.96) | |
| > 36 | 9 | 2 | 1 | 1 | |||
| Educational Level | MSC | 84 | 102 | 0.077 | 1.9(0.932,3.873)1 | 0.034** | 2.35(1.065,5.179) |
| BSC | 13 | 30 | 1 | 1 | |||
| Equipment | No | 5 | 18 | 0.042 | 0.34(0.123,0.962) | 0.126 | 0.41(0.132,1.29) |
| Yes | 92 | 114 | 1 | 1 | |||
| Guideline | No | 68 | 110 | 0.019 | 0.45(0.25,0.882) | 0.006** | 0.4(0.19,0.75) |
| Yes | 29 | 22 | 1 | 1 | 1 | 1 | |
Factors associated with Attitude towards endotracheal suctioning
In this study, few variables, such as sex, educational status, availability of equipment and training were selected for multivariable analysis using binary logistic regression with a p-value less than 0.25. In the final multivariable logistic regression analysis, educational status and training of nurses working in ICU were linked with knowledge of endotracheal suctioning, as show in the table 9, ICU nurses with a master’s degree were five times more likely to possess a positive attitude towards endotracheal suctioning compared to those with a Bachelor degree [AOR=4.84; 95%CI: 1.842, 12.842]. Additionally, ICU nurses who did not receive training on endotracheal suctioning were 84% less likely to hold a positive attitude towards this procedure compared to their trained counterparts [AOR=0.16; 95%CI: 0.085, 0.297].
Table 9: Factors associated with level of Attitude among nurses working in ICU, Addis Ababa, Ethiopia (n=229)
| Variable | Categories | Attitude | P-value
| COR
| P- value
| AOR
| |
| Negative | Positive | ||||||
| Sex | Female | 34 | 63 | 0.176 | 0.7(0.4,1.182) | 0.336 | 0.74(0.4,1.366) |
| Male | 58 | 74 | 1 | 1 | 1 | 1 | |
| Educational status | MSC | 86 | 100 | 0.004 | 5.3(2.136,13.168) | 0.002** | 4.84(1.824,12.824) |
| BSC | 6 | 37 | 1 | 1 | 1 | 1 | |
| Availability of Equipment | No | 6 | 17 | 0.153 | 0.5(0.186,1.3) | 0.338 | 0.59(0.195,1.752) |
| Yes | 86 | 120 | 1 | 1 | 1 | 1 | |
| Training | No | 38 | 112 | 0.003 | 0.2(0.086,0.3}1 | 0.001** | 0.16(0.085,0.297) |
| Yes | 54 | 25 | 1 | 1 | 1 | 1 | |
Discussion
The purpose of this study was to assess Knowledge, Attitude and practice of endotracheal tube suctioning and associated factors among Intensive care unit Nurses in Selected Public Hospitals in Addis Ababa. This is because; knowing the levels of knowledge, attitude, practice, and associated factors towards endotracheal suctioning is a cornerstone for the management and control of the morbidity and mortality associated with errors and harms during medical care services.
The present study showed that the nurses’ level of good knowledge towards endotracheal suctioning was 51.5%. The present study finding was lower when compared with a study conducted in selected hospitals in Der Salam, Tanzania hospital, which reported the knowledge of nurses towards endotracheal suction 80.6% [12]. The variation might be due to that the differences in socio-economic characteristics. The present study finding was higher compare to the study done in tertiary hospitals in Karachi, Pakistan which reported the self- rated good level of knowledge on tracheostomy care was 40% [29]. The variation might be due to that the difference in the study population. A study conducted in Karachi tertiary Hospital, on tracheostomy care while the present study was conducted on endotracheal suctioning.
The present study finding was consistent with the study conducted in at two teaching hospitals, Bhagalpur, Nepal which reported the self- rated good level of knowledge on endotracheal suctioning 55.8% [16].
The present study showed that the nurse’s level of good practice towards endotracheal suction was 42.4%. The present study finding was consistent with the study conducted in at two teaching hospitals, Bhagalpur, Nepal which reported the self- rated good level of practice on endotracheal suctioning 44.4% [16].
The present study finding was higher than the study conducted in Amhara region public Hospital where the ICU nurses on endotracheal suctioning was 28.9% [14]. The variation might be due to that the difference in sample size. The present study finding was also lower than the study conducted in Khartoum teaching hospital Sudan, where the level of practice of endotracheal suction was 76.8% [22]. The possible justification might be due to that the differences in sample size and study setting.
The present study showed that the nurse’s level of positive attitude towards endotracheal suctioning was 40.2%. The present study was lower than the study conducted in Himalaya University, India, where the ICU nurses’ attitude towards endotracheal suctioning was 68.466% [39]. This variation may be due study setting and sampling method. The present study finding was also lower than the study conducted in Jordanian hospitals in Al-Karak and the capital, Amman where the level of positive attitude of patient safety was [65%] [40]. This variation may due sample size, sampling method and study setting. In addition, the present study is done on attitude of ICU nurses towards endotracheal suctioning while this study was done on oral care.
The present study finding was consistent with the study conducted in at two public hospital in Amhara region which reported the positive attitude towards endotracheal suctioning 48.9%[14].
Intensive care nurses with age range of 26-30 years are 5 time more likely have good knowledge compared to those ICU nurse with greater than 36 years of age [AOR=4.9; 95%CI: 1, 23.4]. This study is supported by a study done in Malaysia [24]. This is possibly due to recent education, technological adeptness, and active engagement in continuing education compared to their older counterparts aged over 36 years. Similarly, ICU nurses those who had work experience less than five years are less likely to have good knowledge about endotracheal suctioning compared those who had work experience 6-11 years [AOR=0.36; 95%CI: 0.154, 0.82]. This finding was supported by a study conducted in public hospital selected in der Salem Tanzania [12]. This is may be due to accumulated clinical exposure, ongoing professional development, and mentorship, compared to those with fewer than five years of experience.
Intensive care nurses under the age of 25 were 97% less likely to perform endotracheal suctioning compared to those over 36 years old [AOR=0.03; 95%CI: 0.002, 0.05]. This study finding is supported by study done Selected Teaching Hospitals, Bharatpur, Chitwan [23] This could be attributed to their relatively limited clinical experience and possibly being in training or early stages of their nursing careers, where they may not yet have gained proficiency in advanced procedures like endotracheal suctioning. Likewise, ICU nurses aged 26-30 were 88% less likely to engage in this practice compared to their counterparts over 36 years of age [AOR=0.12; 95%CI: 0.023, 0.623]. This study finding is supported by done in Selected Teaching Hospitals, Bharatpur, Chitwan [23]. This may be due to fewer opportunities for exposure and practice in complex procedures early in their careers, combined with potential assignments to less critical roles or patients requiring less intensive care.
Among nurses working in the ICU, those with a Master of Science degree were twice as likely to perform endotracheal suctioning compared to those with a Bachelor of Science degree [AOR=2.35; 95%CI: 1.065, 5.179]. This study finding is supported systematic review done in India [15]. This could be due to possibly indicating that higher education levels provide enhanced knowledge, skills, clinical decision-making abilities, and role expectations conducive to undertaking such advanced procedures.
Nurses working in ICU where guidelines were not available were 60% less likely to perform endotracheal suctioning compared to those in units with guidelines [AOR=0.4; 95%CI: 0.19, 0.75]. This study is similar with study done in Egypt Minia University Hospital [41]. This could be because clear protocols and guidelines provide structured frameworks that enhance nurses' confidence and competence in performing such critical procedures. The absence of guidelines may lead to uncertainty or hesitancy among nurses, impacting their willingness and ability to carry out endotracheal suctioning.
ICU nurses with a Master’s of Science [BSc] degree were five times more likely to possess a positive attitude towards endotracheal suctioning compared to those with a bachelor’s degree [AOR=4.84; 95%CI: 1.842, 12.842]. This study finding is supported by study done in a study conducted in public hospital selected in der Salem Tanzania [12]. This could be attributed to the advanced education and training associated with an MSc degree, which likely enhances their understanding, confidence, and perceived competency in performing complex procedures such as endotracheal suctioning. Additionally, nurses with an MSc degree may have been exposed to more comprehensive coursework or clinical experiences that emphasize the importance and efficacy of such procedures, thereby fostering a more positive attitude towards their execution in critical care settings.
Additionally, ICU nurses who did not receive training on endotracheal suctioning were 84% less likely to hold a positive attitude towards this procedure compared to their trained counterparts [AOR=0.16; 95%CI: 0.085, 0.297]. This study finding is supported by study done the study done in tertiary hospitals in Karachi, Pakistan[29]. This could be because training provides essential knowledge, skills, and confidence necessary for performing the procedure effectively and safely. Without proper training, nurses may feel unprepared or insecure about their abilities, impacting their attitude towards endotracheal suctioning.
Conclusion
In the present study, more than half of the nurses [51.5%] had good knowledge, 57.6% had poor practice and 59.8% had negative attitude towards endotracheal tube suctioning. The multivariable logistic regression analysis showed the age of the nurses and their experience were factors significantly associated with knowledge towards endotracheal suctioning.
Age of the nurse, educational status and availability of guideline in the work unit were factors significantly associated with practice towards endotracheal suctioning. Training and educational status were factors significantly associated with attitude towards endotracheal suctioning. Moreover, the present study offers significant evidence to support other studies, helps in addressing the above-mentioned factors through tailored interventions, and is also essential to improve patient care and outcomes.
Conflicts of Interest:
The author declare no conflicts of interest.
References
-
Hamed EE, Al-Swidan HA, Fadlalmola HA, Alwesabi SA. (2023). Assessment of Nurse’s Knowledge Regarding Endotracheal Tube Suctioning in Intensive Care Units, Najran Hospitals, Saudi Arabia. Int J Nurs Educ. 15(2):12–7. 2. Lamichhane A, Koirala
Publisher | Google Scholor -
Lamichhane A, Koirala D, Thapa B, Silwal M. (2020). Knowledge regarding endotracheal suctioning among Nurses of a teaching hospital of Kaski District. J Gandaki Med Coll. 13(2):178–82.
Publisher | Google Scholor -
Ntelele CT. (2023). Intensive care nurses’ knowledge about endotracheal suctioning guidelines in one major academic hospital in Johannesburg.
Publisher | Google Scholor -
Schults JA, Mitchell ML, Cooke M, Long DA, Ferguson A, Morrow B. (2021). Endotracheal suction interventions in mechanically ventilated children: an integrative review to inform evidence-based practice. Aust Crit Care. 34(1):92–102
Publisher | Google Scholor -
Paramjyothi BB, Daniel LE, Indira S. (2016). A study to assess the knowledge regarding ET suctioning among staff nurses and student nurses in NMCH, Nellore. Int J Appl Res. 2(6):150–2.
--> -
Nasoori M, Pooladi S, Yazdankhahfard M, Mirzaei K. (2023). Investigating the Relationship between the Level of Compliance with Airway Care Standards and Complications from Endotracheal Intubation: A Cross-Sectional Study. J Crit Care Nurs. 16(2):19–28
--> -
Organization WH. Nursing and midwifery in the history of the World Health Organization 1948-2017. 2017;
Publisher | Google Scholor -
Sousa AS, Ferrito C, Paiva JA. (2018). Recommendations for the prevention of adverse events in endotracheal suctioning–Integrative Review. Cad Saúde. 10(1):42–7.
--> -
Elshahat HTM, Kafl RK. (2023). Effect of evidence-based recommendations about open endotracheal suctioning on nurses’ performance at neonatal intensive care units. Assiut Sci Nurs J. 11(35):12–20.
Publisher | Google Scholor -
Heidari M, Shahbazi S. (2017). Nurses’ awareness about principles of airway suctioning. J Clin diagnostic Res JCDR. 11(8):LC17.
Publisher | Google Scholor -
Mohamed H, Mahmoud M, Gouda T, Kandeel N. (2023). Comparison Between the Effect of Open and Closed Tracheal Suction Systems on Physiological Parameters of Critically Ill Patients. Mansoura Nurs J. 10(1):271–82.
--> -
Mwakanyanga ET, Masika GM, Tarimo EAM. (2018). Intensive care nurses’ knowledge and practice on endotracheal suctioning of the intubated patient: A quantitative cross-sectional observational study. PLoS One. 13(8):e0201743.
Publisher | Google Scholor -
Majeed HM. (2017). Assessment of knowledge and practices of intensive care unit nurses about endotracheal suctioning for adult patients in Baghdad teaching hospitals, Iraq. Int J Res Med Sci. 5(4):1396–404.
Publisher | Google Scholor -
Pinto HJ, D’silva F, Sanil TS. (2020). Knowledge and Practices of Endotracheal Suctioning amongst Nursing Professionals: A Systematic Review. Indian J Crit Care Med peer-reviewed, Off Publ Indian Soc Crit Care Med. 24(1):23–32.
--> -
Afenigus AD, Mulugeta H, Bewuket B, Ayenew T, Getnet A, Akalu TY, et al. (2021). Skill of suctioning adult patients with an artificial airway and associated factors among nurses working in intensive care units of Amhara region, public hospitals, Ethiopia. Int J Africa Nurs Sci. 14.
Publisher | Google Scholor -
Shrestha S, Shrestha R. (2018). Knowledge and Practice Regarding Endotracheal Suctioning among Nurses of Selected Teaching Hospitals, Bharatpur, Chitwan. Acta Sci Med Sci. 2(6):10–6.
Publisher | Google Scholor -
Day T, Farnell-Ward S, Wilson-Barnett J. (2022). Suctioning: A review of current research recommendations. Intensive Crit Care Nurs. 18:79–89.
Publisher | Google Scholor -
Aboalizm SE, Abd Elhy AH. (2019). Effect of Educational Intervention on Nurses’ Knowledge And Practices Regarding Endotracheal Tube Suctioning. Int J Nurs Heal Sci. 5(3):1–8.
Publisher | Google Scholor -
Rad LL, Carter B, Curley MAQ, Copnell B, Tume LN. (2021). Is paediatric endotracheal suctioning by nurses evidence based? An International Survey. Nurs Crit Care. 26(5):372–9.
Publisher | Google Scholor -
Gilder E, Parke RL, Jull A. (2019). Endotracheal suction in intensive care: A point prevalence study of current practice in New Zealand and Australia. Aust Crit Care. 32(2):112–5.
Publisher | Google Scholor -
Elsaman SE. (2017). Effect of Application of Endotracheal Suction Guidelines on Cardiorespiratory Parameters of Mechanically Ventilated Patients. IOSR J Nurs Heal Sci. 06(01):41–8.
Publisher | Google Scholor -
Elbokhary R, Osama A, Al-Khader M. (2015). Knowledge and practice of ICU nurses regarding endotracheal suctioning for mechanically ventilated patients in Khartoum Teaching Hospital. Am J Clin Neurol Neurosurg. 1(2):92–8.
--> -
Shrestha S, Shrestha R. (2018). Knowledge and Practice Regarding Endotracheal Suctioning among Nurses of Selected Teaching Hospitals, Bharatpur, Chitwan.
Publisher | Google Scholor -
Afandi AN, Ludin SM. (2020). Icu Nurses’ Perceived Knowledge, Attitude, and Practiceon Endotracheal Suctioning: a Preliminary Study Atahospital in Pahang, Malaysia. Malaysian J Med Res. 4(4):23–8.
--> -
Bülbül Maraş G, Kocaçal Güler E, Eşer İ, Köse Ş. (2017). Knowledge and practice of intensive care nurses for endotracheal suctioning in a teaching hospital in western Turkey. Intensive Crit Care Nurs. 39:45–54.
Publisher | Google Scholor -
Lin YS, Chang JC, Chang TH, Lou MF. (2011). Critical care nurses’ knowledge, attitudes and practices of oral care for patients with oral endotracheal intubation: A questionnaire survey. J Clin Nurs. 20(21–22):3204–14.
Publisher | Google Scholor -
Varghese S, Moly K. (2016). Exploratory study on the knowledge and skill of critical care nurses on endotracheal suctioning. J Natl Accredit Board Hosp Healthc Provid. 3(1):13.
Publisher | Google Scholor -
Zeb A. (2017). Knowledge and Practice of ICU Nurses Regarding Endotracheal Suctioning in Tertiary Care Hospitals, Peshawar. JOJ Nurs Heal Care. 6;2
Publisher | Google Scholor -
Fauzia Rafiq, Badil, Hussain M, Saeed MFS, GUR. (2022). Intensive Care Nurses’ Knowledge and Practice of Endotracheal Suctioning Intubated Patients in Tertiary Care Public Sector Hospitals in Karachi, Pakistan. Pakistan J Heal Sci.128–32.
--> -
Jin X. (2011). ICU Nurses’ Knowledge and Attitude about Endotracheal Suctioning of Mechanically Ventilated Patients with Artificial Airways. In 2011.
--> -
Azizian K, Azadi A, Veisani Y, Bastami M. (2020). The effect of performance feedback and educational video on endotracheal-suctioning practices of critical care nurses. J Educ Health Promot. 9:112.
Publisher | Google Scholor -
Leddy R, Wilkinson JM. (2015). Endotracheal suctioning practices of nurses and respiratory therapists: How well do they align with clinical practice guidelines? Can J Respir Ther CJRT = Rev Can la Ther Respir RCTR. 51(3):60–4.
Publisher | Google Scholor -
Lai J, Brettle A, Zhang Y, Zhou C, Li C, Fu J, et al. (2022). Barriers to implementing evidence-based nursing practice from the hospitals’ point of view in China: A regional cross-sectional study. Nurse Educ Today. 116:105436.
Publisher | Google Scholor -
Haghighat S, Yazdannik A. (2015). The practice of intensive care nurses using the closed suctioning system: An observational study. Iran J Nurs Midwifery Res. 20(5):619–25.
Publisher | Google Scholor -
Satirapoj B, Adler G. (2015). Prevalence and Management of Diabetic Nephropathy in Western Countries. 90502:61–70.
Publisher | Google Scholor -
Werke EB, Weret ZS. (2023). Occupational stress and associated factors among nurses working at public hospitals of Addis Ababa, Ethiopia, 2022; A hospital based cross-sectional study. Front Public Heal. 11(April).
Publisher | Google Scholor -
Ansari A, Alavi N, Adib-Hajbaghery M, Afazel M. (2011). The gap between knowledge and practice in standard Endo-tracheal suctioning of ICU nurses, Shahid Beheshti Hospital. Iran J Crit Care Nurs. 30;5.
Publisher | Google Scholor -
Sunny MS, rani DSRR, rani DSRR, rani DSRR. (2021). Nurses’ Knowledge and Attitude on Practice of Artificial Airway Suctioning. Res Reserv. 7(1).
Publisher | Google Scholor -
Ayyad A, Baker NA, Oweidat I, Al-Mugheed K, Alsenany SA, Abdelaliem SMF. (2024). Knowledge, attitudes, and practices toward Patient Safety among nurses in health centers. BMC Nurs. 23(1):171.
--> -
Mohamed S. (2022). Effect of Clinical Guidelines About Endotracheal Tube Suctioning on Nurses’ Knowledge and Practice at Neonatal Intensive Care Unit. Assiut Sci Nurs J.
Publisher | Google Scholor
