RESEARCH ARTICLE
1Department of Community Medicine, University of Port Harcourt Teaching Hospital, Rivers State.
2Department of Community Health, University of Benin Teaching Hospital, Edo State.
*Corresponding Author: aEnuagwuna F.C1
Citation:
aEnuagwuna F.C1, (2024) *, Estimating health care cost and effects among urban households in Rivers State Nigeria
1(1). Global Journal of Infectious Diseases and Health Insight (GJIDHI) DOI: https://doi.org/10.64347/3064-707X/GJIDHI.001
Copyright: © (2024) aEnuagwuna F.C1*, this is an open-access article distributed under the terms of The Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Received: February 01, 2024 | Accepted: March 09, 2024 | Published: March 18, 2024
Abstract
Background: Most health systems are confronted with high demand but have limited budgets with which to provide necessary services. The cost of obtaining healthcare continues to be a major challenge in low- and middle-income countries due to low health insurance coverage. The aim of this study was to estimate the cost of healthcare and its effects on urban residents in Rivers State.
Methods: This community-based descriptive cross-sectional study was conducted among 624 respondents residing in Urban settlements in Rivers State who were recruited using a multi -stage sampling technique. Data was obtained using a semi-structured interviewer-administered questionnaire. IBM Statistical Product and Service Solution version 25 was used to analyse the data
Results: The respondents in the Urban region of Rivers State Nigeria spend an average of $90.7 on healthcare,16.3% experienced catastrophic health expenditure with 12.7% living below the poverty line following healthcare expenditure in the past year. The residents experience several consequences of healthcare cost ranging from sacrificing money meant for other needs to pay for healthcare, selling of assets, having their wards drop out of school, borrowing and death of loved ones.
Conclusion: The cost of obtaining healthcare among urban residents appears to be on the high side, due to the various direct medical and non-medical cost that accompanies the process of accessing healthcare. A community-based insurance scheme will alleviate the suffering due to the high cost of healthcare among residents in urban communities in Rivers State.
Keywords: Healthcare Cost, Consequences, Urban areas, Rivers State
Introduction
Health care expenditures often place a burden on the financial sustainability of households particularly in resource-poor settings where effective coverage of health insurance schemes are lacking and out-of -pocket (OOP) expenditure is the common form of health care financing (1). Out-of -pocket health expenditure has been shown to have a negative impact on health equity, and healthcare utilization and may lead to catastrophic spending. Catastrophic costs due to healthcare refer to households spending more than a stated percentage threshold of 10% of their household income (2). Healthcare expenditure may occur through combinations of direct and indirect taxation; voluntary/non-voluntary prepayment and/or co-payment or co-insurance, or through direct out-of-pocket payment by care-seekers at the point of care. These different means of health financing offer different levels of financial risk protection, access and quality of care for users (2,3).
Globally, approximately 44 million households or more than 150 million individuals, face catastrophic health expenditure (CHE), and about 25 million households or more than 100 million individuals are forced into poverty due to the need to pay out of pocket for healthcare services every year (3).
The impact of out-of-pocket payments for healthcare is beyond catastrophic expenditure alone Expenditures on health can be financially disastrous for poor households as many people in need of healthcare, particularly the poor, may not utilize health services, some may patronize low-quality healthcare simply because they cannot meet the direct medical and non-medical costs of healthcare services (3).
Some of the coping strategies for payment of health expenditures include households being able to manage payments by selling off assets, borrowing and reduction in household consumption which are all likely to have adverse effects on their wellbeing (4,5).
The exceptionally low health insurance coverage in Nigeria about 2.5% of the population and an even lower percentage of the population in Rivers State (l1ess than 2%) that is covered by any form of pre-payment and risk pooling scheme expose a greater percentage of the population to out of pocket payment and catastrophic health expenditures (4,5).
Household healthcare expenditure considering the various costs of healthcare has not been fully assessed among households living in urban communities in Rivers State. Most studies only focused on the catastrophic health payment. There is therefore need to highlight the various costs of healthcare and the its consequences among urban residents in Rivers State.
Methods
Study Area
This study was conducted in Rumueme in Obio/Akpor LGA and Borokiri in Port Harcourt LGA of Rivers State, which is situated in the oil-rich Niger Delta region of Nigeria. Out of 23 local government areas (LGAs) in the state, Port Harcourt City and Obio-Akpor LGAs, are considered to be predominantly urban. Port Harcourt being the capital city, more developed and largely occupied by political appointees, high-grade civil servants and large-scale businessmen. While Obio-Akpor is less developed and is mainly occupied by low and intermediate-grade civil servants, businessmen and farmers.
The public and private sectors are involved in providing orthodox healthcare services in Rivers State. There are five tertiary healthcare facilities providing specialist services in Port Harcourt. One is owned by the federal government while the other four are state-owned. They include the Rivers State University Teaching Hospital (RSUTH) (former Braithwaite Memorial Specialist Hospital), Professor Kelsey Harrison Hospital, Neuro-psychiatric Hospital, Dental & Maxillofacial Hospital and University of Port Harcourt Teaching Hospital (UPTH
Study Design
The study was a community-based descriptive cross-sectional study using mixed methods of data collection techniques
Study Population
The study population comprised households normally residents within each of the two urban Local Government Areas in Rivers State for up to one year before the commencement of the study; a period sufficient enough for one to require medical care
The study population of the focus group discussions comprised the head of households, whose households experienced Catastrophic health expenditure in the last year.
Sample Size Estimation
The sample size was estimated using Cochran’s formula for calculating sample size for a descriptive study with a single proportion
n =
Were n= the minimum sample size, Z= the standard normal deviate corresponding to the level of significance; Z=1.96,
P= The prevalence of CHE in a previous study, 32.8% (6).
q= 1-p = 0.6,
e= Level of precision or maximum error of estimate at 95% Confidence Level, e=0.05.
A study design effect of two was applied, making the minimum sample size required to be 608. The sample size of the focus group discussions comprised 49 heads of households who experienced Catastrophic health expenditure
Sampling Method
The households were selected by a multi-stage sampling technique that involved the selection of two communities from Rivers State urban LGAs (Port Harcourt city LGAs, Obio/Akpor LGAs,) A simple random sampling method, using balloting was applied to select one ward each from the 17 wards in Obio/Akpo and the 20 wards in Port Harcourt LGAs. The second stage was the selection of communities using a simple random sampling by balloting, Rumueme was selected out of 7 communities in ward 11 of Obio/Akpor and Borokiri was selected from 14 communities in ward 7 of Port Harcourt LGA. The third stage was the selection of households from each of the communities using a cluster sampling method, Houses were divided into three clusters using major streets as landmarks and one out of the three clusters and households living in the selected clusters were interviewed. A purposive sampling method was used to select 49 heads of households who experienced catastrophic health expenditure for the focus group discussions
Study Instrument was semi-structured structured questionnaire adapted from valid existing instruments that have been used in related investigations (7,22). The questionnaire was programmed in the open data kit application (ODK). It was interviewer-administered in simple English language, but the interviewer may decide to relay it in pidgin English depending on the educational level of the respondent and has five subsections. Healthcare cost for multiple episodes of illness was determined by asking questions on the amount spent on various direct medical and direct non-medical costs in addition to making reference to receipt of payment made for healthcare. Costs associated with consultations, medications, tests, and admissions/hospital stays incurred during the past one year are considered direct medical costs, an estimate of direct non-medical costs was made, including the price of travel [to and from the hospital], meals consumed while visiting, and lodging.
A Focus group discussion guide was used to conduct the FGD were a total of 49 heads of households were purposively selected for the discussions. Data saturation was reached after four sessions in Rumueme community in OBALGA and three sessions in Borokiri community in PHALGA with seven participants each. FGD was conducted with the help of two research assistants. A voice recorder was used to record the sessions
Instrument validity
The questionnaire was pre-tested among 61 heads of households which is 10% of the estimated sample size in Akpajo community in Eleme LGA, which is not part of the study area, to ensure consistency and reliability of the instrument. The instrument was then updated based on the limitations observed during the pretesting
Data Analysis
Data was analyzed using IBM Statistical Product and Service Solution version 25. Variables were summarized as means, median and standard deviation for continuous variables while categorical variables were summarized as frequency distribution tables and charts. Direct medical cost include cost of consultation, drugs, investigations and admission/hospital stay within the previous year. Estimation of direct non-medical costs which include cost of travel (transportation to and from the hospital), meals taken during hospital visits and accommodation.
Qualitative Data Management
Audio recordings of the focus group discussions were transcribed into Microsoft word documents. The transcriptions were then uploaded into Atlas Ti. Version 8, and a content analysis approach was used to analyze the data, aiming to describe the personal experiences of participants concerning costs and payments for healthcare. The principal researcher and an assistant read the first three transcripts and inductively developed codes which were recorded in a book. The researchers then read the remaining four transcripts independently, applying the already identified codes. They compared and discussed their reviews and in instances where new codes were identified, they made a decision on adding new codes to the existing codes. The final codes were entered into the coding database and analyzed with the corresponding quotations. The results were presented as diagrams, quotation tables and code frequency tables
Ethical Considerations
The University of Port Harcourt Teaching Hospital Ethics Committee granted approval for the study [UPTH/ADM/90/S. II/VOL.XI/1111]. Written informed consent was obtained from the participants before the study commenced. The researcher was the only one with a passcode to the password-protected computer where the data was kept. Written informed consent was also obtained from the participants in the FGDs. Permissions was obtained to record the sessions with a voice recorder. The audio recordings were saved on a personal computer only accessible to the researcher and the results and outcomes of the study shared with them
Study duration
The study duration was from February 2020 to January 2023
Results
Table I: Social Demographic Characteristics
| Variable | Frequency n=624 | Percent (%) |
| Sex | ||
| Males | 621 | 99.5 |
| Females | 3 | 0.5 |
| Marital status | ||
| Single | 7 | 1.1 |
| Married | 431 | 69.1 |
| Separated | 63 | 10.1 |
| Divorced | 43 | 6.9 |
| Widowed | 48 | 7.7 |
| Cohabiting | 32 | 5.1 |
| Education | ||
| No formal education | 19 | 3 |
| Primary | 19 | 3 |
| Secondary | 258 | 41.3 |
| Tertiary | 328 | 52.6 |
| Spouse education n=463 | ||
| No formal education | 6 | 1.3 |
| Primary | 14 | 3 |
| Secondary | 282 | 60.9 |
| Tertiary | 161 | 34.8 |
| Occupation | ||
| Senior public servants, managers, large scale traders, businessmen | 19 | 3 |
| Intermediate grade public servants and senior school teachers | 217 | 34.8 |
| Junior school teachers, professional drivers, artisans | 340 | 54.5 |
| Unemployed, students, subsistence farmers | 39 | 6.3 |
| Others | 9 | 1.4 |
Table I shows that 621(99.5%) respondents were males, while 3(0.5%) respondents were females. The description of the marital status shows that 431(69.1%) respondents were married, 63(10.1%) respondents were separated, 48(7.7%) respondents were widowed, 43(6.9%) respondents were divorced and 7(1.1%) respondents were single. In terms of education, 328(52.6%) of the respondents had tertiary secondary education, 258(41.3%) had secondary education, 19(3.0%) had primary education and 9(3.0%) of the respondents had no education. Furthermore, the table shows that 340(54.5%) respondents were junior school teachers, professional drivers and artisans, 217(34.8%) respondents were intermediate grade public servants and seniors school teachers, 39(6.3%) respondents were unemployed and 19(3.0%) of the respondents were senior public servants, large scale traders and businessmen.
Table II: Source of money for treatment by respondents
| Source | Frequency n=624 | Percent (%) |
| Personal income | 316 | 50.6 |
| Sourced for loans | 142 | 22.8 |
| Friends | 199 | 31.9 |
| Relatives | 181 | 29 |
| Employer | 81 | 13 |
| Sales of properties | 31 | 5 |
| Contribution from community | 13 | 2.1 |
Table II shows that source of money for treatment was from personal income in 316(50.6%) of the respondents, 228(36.5%) sourced for loans, 199(31.9%) of the respondents got money from friends, and 181(29.0%) received money from relatives. Other sources were employer 81(31.0%), sales of properties 31(5.0%) and contribution from communities 13(2.1%).
Table III: Direct and Indirect cost of acquiring healthcare
| Variable | Mean | Standard deviation | $ |
| Transport | 5896.3 | 12173.5 | 9.1 |
| Feeding | 10613.3 | 18260.3 | 16.3 |
| Admission/Accommodation | 29481.3 | 60867.6 | 45.4 |
| Drugs | 11792.5 | 24347.1 | 18.1 |
| Card | 1179.3 | 2434.7 | 1.8 |
| Direct non-medical cost | 16509.5 | 30433.8 | 25.4 |
| Direct medical cost | 42453.1 | 87649.4 | 65.3 |
| Total cost of healthcare | 58962.7 | 118083.2 | 90.7 |
Table III shows that the respondents spend an average of N5896.3±12173.5 on transportation, N10613.3±18260.3 on feeding, N29481.3±60867.6 on admission, N11792.5±24347.1 on drugs, and N1179.3±2434.7 on cards. Also, the average direct non-medical cost was N16509.5±30433.8, the average direct medical cost was N42453.1±87649.4 and the average total cost of obtaining care was N58962.7±118083.2.
Table IV: Effects of health care payment and guide to the choice of treatment
| Variable | Frequency n=624 | Percent (%) |
| Sacrificed school fees or feeding for healthcare | ||
| Yes | 163 | 26.1 |
| Sold assets for healthcare expenditure | ||
| Yes | 55 | 8.8 |
| School dropout due to healthcare expenditure | ||
| Yes | 22 | 3.5 |
| Cannot afford some treatment options | ||
| Yes | 131 | 21.0 |
| What guides choice of treatment | ||
| Money | 558 | 89.4 |
| Doctor’s decision | 50 | 8.0 |
| Family’s decision | 16 | 2.6 |
| Borrowed money because of medical treatment | ||
| Yes | 142 | 22.8 |
| Where did you borrow from n=142 | ||
| Corporative society | 19 | 13.4 |
| Church | 21 | 14.8 |
| Family | 35 | 24.6 |
| Bank | 42 | 30.0 |
| Friends | 49 | 34.5 |
Table IV shows that 163(26.1%) respondents sacrifice money meant for school fees for health care, 55(8.8%) sold their assets, 22(3.5%) had school dropout, 131(21.0%) could not afford some treatment options and 142(22.8%) borrowed money to pay for health care.
V: Impoverishing effects of healthcare expenses and guide to the choice of treatment in the two LGA
| Variable | PHA LGA n=312 | OBA LGA n=312 |  (p-value) (p-value) |
| Sacrificed school fees or feeding for healthcare | |||
| Yes | 96(30.8) | 67(21.5) | 6.984(0.008)* |
| Sold assets for healthcare expenditure | |||
| Yes | 43(13.8) | 12(3.8) | 19.162(<0> |
| Able to pay for admission | |||
| Yes | 210(67.3) | 141(45.3) | 31.004(<0> |
| Income | |||
| < 100000> | 73(18.4) | 324(81.6) | 23.369(<0> |
| >100000 | 29(12.8) | 198(87.2) | |
| What determines your choice of treatment | |||
| Money | 289(92.6) | 269(86.2) | 8.717(0.013)* |
| Doctor’s decision | 15(4.8) | 35(11.2) | |
| Family’s decision | 8(2.6) | 8(2.6) | |
| Borrowed money because of medical treatment | |||
| Yes | 108(34.6) | 34(10.9) | 49.924(<0> |
Table V shows that 96(30.8%) respondents in PHALGA and 67(21.5%) respondents in OBALGA had sacrificed school fees or feeding for healthcare payment (X2=6.984, p=0.008), 43(13.8%) of the respondents in PHALGA and 12(3.8%) of the respondents in OBALGA had sold assets for healthcare expenditure (X2=19.162 p<0 X2=31.004, X2=23.396,>
Figure I shows that majority of the participants articulated that the cost of healthcare was high in Rivers State, other participants were of the opinion that the cost of healthcare in Rivers State is not favorable, or affordable for the common man while a few felt the cost of healthcare came with financial strain. Only one participant indicated that the cost of healthcare was fair
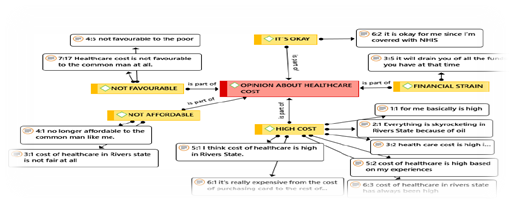
Figure I: Opinion about health care cost
Figure 2 shows that most of the respondents were above the poverty line, 79(12.3%) of the study population were below the World Bank poverty line
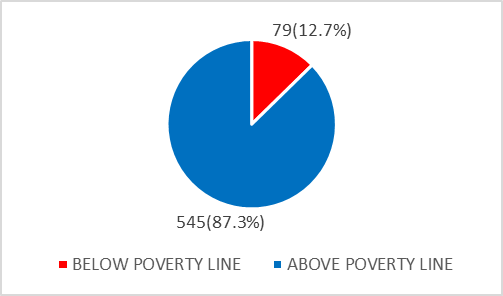
Figure 2: Poverty line graph using $3.20 for low-income countries 26.
Table VI: Experience relating to paying for healthcare
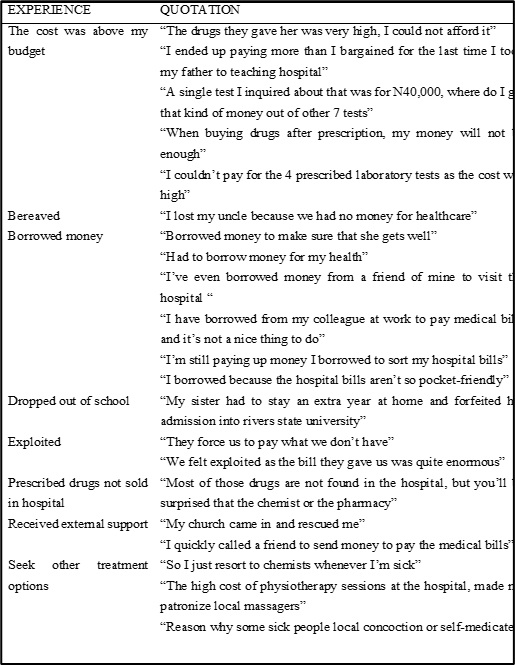
Table VI shows Focus group discussion experience relating to paying for healthcare, “The drugs they gave her was very high, I could not afford it” “I ended up paying more than I bargained for the last time I took my father to teaching hospital” “A single test I inquired about that was for N40,000, where do I get that kind of money out of other 7 tests” “When buying drugs after prescription, my money will not be enough” “I couldn’t pay for the 4 prescribed laboratory tests as the cost was high”
Table VII: Catastrophic head count, poverty head count and Impoverishment Estimates ($ =N411.19)
| Catastrophic payment measure | Threshold |
| 10% household income | |
| Catastrophic head count (H) | 16.3% |
| Poverty head count (%) | 12.7% |
Table VII shows that 16.3% of the respondents spent 10% or more of their household income on healthcare expenditure, catastrophic overshoot of 28.1% and poverty head count of 12.7%
Discussion
In an attempt to access health care services, the respondents spend as much as N5896.3±12173.5 ($9) on transportation. This may be due to hike in transportation fares due to the cost of obtaining premium motor spirit (7,8). Despite the unevenly geographical location distribution in healthcare service between urban and rural residents, urban residents still spend a lot on transportation to access health care services (9,10). The goal of ensuring universal health coverage may be far from being achieved among urban residents in Rivers State especially as it pertains to obtaining specialized healthcare services due to the cost of transportation (11). The distance to health care facilities has necessitated some of the respondents to seek accommodation in the health facilities with a resulting effect of spending as high as 29481.3±60867.6 ($45.4) for admission/accommodation expenses. This may have further worsened the burden on the respondents, This average cost of admission/accommodation was far higher than what was reported in previous studies (12), although the latter may not have considered the cost of accommodation for relatives and caregivers. According to previous studies in the United States, reducing the length of stay in hospital has a significant impact on the reduction of the cost of obtaining healthcare among patients discharged from an academic medical center (12).
A major component of the cost of obtaining health care is the cost of feeding. Patients and their caregivers often spend a lot on feeding during the period they access care; this is one aspect that has been neglected because it is not a direct medical expense and is rarely included as part of the package in most health insurance schemes (13,14). In this study, as high as 10613.3±18260.3 ($16.3) was spent on the average by the respondents during the health care visits.
Drug cost amounted to an average of $18 among urban residents. This is on the high side considering that most of the payments were made out of pocket because most of the population are not enrolled in the National Health Insurance Authority scheme. The cost of obtaining drugs has also been reported as a barrier to accessing healthcare services in previous findings in Nigeria (15,16).
The residents in urban area of Rivers State spend an average of 16509.5±30433.8 ($25.4) on direct non-medical costs. A similar observation was reported among patients in Northern Nigeria (17). This may affect the health-seeking behaviour of urban residents because they have to make provision for all the various direct non-medical cost in addition to the direct medical cost, they may incur from treatment directly. The average direct medical cost amounted to 42453.1±87649.4 ($65). The total cost of healthcare was estimated to be was N58962.7±118083.2. ($90.7) which seems to be on the high side for a country where the minimum wage is about $50 (18) and close to 40% of the population are poor, urgent attention is needed in the health sector (19).
The majority of the participants in the Focus Group Discussions articulated that the cost of healthcare was high in Rivers State, other participants believed that the cost of healthcare in Rivers State is not favorable, or affordable for the common man while a few felt the cost of healthcare came with financial strain. The participants felt that the cost of health care in River state was high and they can barely afford it. They believed the high cost of living in the state triggered the cost of health care. Most of them paid for health at the point of seeking care. Which may not be available at the point of need. Only one participant indicated that the cost of healthcare was fair. Considering that a lot of the respondent’s spouses were students and unemployed much of the burden of paying for health care will lie on the heads of the household. Which may not be readily accessible at the time of emergency.
A lot of urban residents have faced some hardship due to cost of health care, such as spending money meant for the tuition fees of their wards on healthcare and borrowing, this corroborate with the finding in a similar study done in selected healthcare facilities in Ile-Ife South-Western Nigeria (7). Some of the respondents could not afford some treatment options that were prescribed by the physicians, the implication is that they may forgo the treatment thereby resulting to more suffering of the sick persons or they may opt for less effective medication which may take longer duration for the sick persons to recover. A similar consequence was reported in a study done among Rural and Urban Households in Oyo State South-Western Nigeria (2). The study showed that 16.3% (102) of the study participants spent more than 10% of their total income on healthcare expenditure, hence falling into catastrophic health expenditure and 79(12.7%) pushed below the world bank poverty line, this could be attributed to the mode of payment for healthcare which is out-of-pocket payment because some of the residents in the urban area had to sell their properties to pay for healthcare. Some of the respondents had to secure loan to off-set healthcare cost, this is consistent with the finding from previous study (2,7,24).
The choice of treatment is meant to be based on the physicians’ prescriptions and recommendations, that is not however the case among urban residents in Rivers State, a lot of them considers the cost of obtaining treatment before they accept the
Limitation of the study
This study did not describe the cost based on the nature of the healthcare needs. Cost of healthcare was assessed generally and this may not highlight the medical conditions that led to more costs of obtaining care. The study was prone to recall bias because the respondents had to recall expenses made up to one year prior to the interview. However, efforts were made to validate claims through repeating of questions to ensure consistency of response and reference to payment receipts when necessary. The data collection protocol provided for extensive documentation of health events as well as incomes and expenditure of households.
Study Implications
The risk of CHE among urban household is high and this is mainly attributed to near absence of financial risk protection in the event of illness episodes, low socio-economic status and high number of dependents. Achieving universal health coverage in urban communities in Rivers State remains a mirage if concerted efforts are not made to address issues related to financial risk protection. This is of note among rural communities with low socio-economic status, high dependency ratio with the main mode of payment for health care being out-of-pocket at the point of access (6). Strategic options for changing this situation are the implementation of the Rivers State contributory health protection programme (RIVCHPP) which has immense potential to offering financial protection to resident to access health services thereby improving the chances of attaining universal health coverage. Further studies should probe into the consequence of out-of-pocket payment for health care in Rural Areas of Rivers State as there is evidence that out-of-pocket payment increases the risk of CHE among households with pediatric emergencies, acute illnesses in adults requiring hospitalization, household receiving essential obstetric care, and those with long-term medical conditions (6,23). Regarding financial barriers, in addition to ensuring the availability of tax-financed, social assistance programmes, Participation in social insurance schemes can also be improved by offering subsidies to those living in poverty. The hidden costs of participation to accessing social protection programmes in general can be lowered by simplifying administrative procedures. A key policy area to reduce both rural poverty and inequalities is social protection. There is ample evidence of the positive impact of social protection on poverty and inequality reduction as well as on its ability to promote inclusion. Access to regular and adequate social protection benefits, prevents poverty and reduces vulnerability through the lifecycle. It reduces the need to rely on negative coping strategies such as pulling children out of school or selling assets when households face economic shocks (25).
Conclusion
The residents of urban region in Rivers State are far from achieving universal healthcare. The various direct medical and direct non-medical costs still limit the residents from fully accessing and utilizing various healthcare services. In a country with low health insurance coverage, more effort is needed to achieve universal health coverage, government needs to increase funding of the healthcare system in addition to widening the coverage of the health insurance Authority. These actions need to be taken quickly to avert the occurrence of catastrophic healthcare payments and reduce the sufferings of residents in Urban communities in Rivers State. Health insurance Authority needs to include direct non-medical costs to their premium package because a lot of patients incur high amounts of direct non-medical costs in an attempt to access healthcare. The situation may be more worrisome in the rural areas, hence there is need to replicate this study among rural residents in Rivers State
Conflict of Interest:
None
Authors’ contributions
All authors were involved in planning and implementation of the study. Data collection team was led by EFC.
Acknowledgement
We are grateful to the communities’ leaders and heads of households. The authors did not receive any funding.
References
-
Onwujekwe O, Okereke E, Onoka C, Uzochukwu B, Kirigia J, Petu A. Willingness to pay for community-based health insurance in Nigeria: do economic status and place of residence matter? Health Policy Plan. 2010 Mar 1;25(2):155-61. DOI: 10.1093/heapol/czp046
Publisher | Google Scholor -
Ilesanmi OS, Adebiyi AO, Fatiregun AA, Ishola I. Consequences of Health Expenditure among Rural and Urban Households in Oyo State, Nigeria. Int J Manag Stud Res. 2020;8(9):8–17. DOI: 10.20431/2349-0349.0809002
--> -
Pyakurel P, Tripathi JP, Myo MM, Acharya B, Pyakurel U, Singh SB,…et al. Catastrophic health expenditure among industrial workers in a large-scale industry in Nepal, 2017: a cross-sectional study. BMJ open. 2018; 8(11): 3-10 DOI: 10.4103/ijoem.IJOEM_168_17
Publisher | Google Scholor -
National Population Commission. Federal Republic of Nigeria, Abuja Nigeria: Nigeria Demographic and Health Survey 2013. Rockville (MD): ICF International. 2014:3-51 https://dhsprogram.com/pubs/pdf/fr293/fr293.
Publisher | Google Scholor -
Russell S. The Economic Burden of Illness for Households in Developing Countries: A Review of Studies Focusing on Malaria, Tuberculosis, and Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome. In: The Intolerable Burden of Malaria II: What’s New, What’s Needed: Supplement to Volume 71(2) of the American Journal of Tropical Medicine and Hygiene [Internet]. American Society of Tropical Medicine and Hygiene; 2004 https://www.ncbi.nlm.nih.gov/books/NBK3768/
Publisher | Google Scholor -
Daprim Samuel Ogaji, Adesina AD. The predictors of catastrophic health expenditure among households in Yenagoa, Bayelsa State. Niger Delta Med J. 2018;2(1):9–23. https://ndmjournal.org/wp-content/uploads/2018/06/Ogaji.
Publisher | Google Scholor -
Okediji PT, Ojo AO, Ojo AI, Ojo AS, Ojo OE, et al., The economic impacts of chronic illness on households of patients in Ile-Ife, South-Western Nigeria. Cureus. 2017(10):3-20 DOI: 10.7759/cureus.1756
Publisher | Google Scholor -
Basu J. Research on Disparities in Primary Health Care in Rural versus Urban Areas: Select Perspectives. Int J Environ Res Public Health. 2022 Jun 10;19(12):7110. DOI: 10.3390/ijerph19127110
Publisher | Google Scholor -
Silal SP, Penn-Kekana L, Harris B, Birch S, McIntyre D. Exploring inequalities in access to and use of maternal health services in South Africa. BMC Health Serv Res. 2012 May 21;12(1):120. DOIhttps://doi.org/10.1186/1472-6963-12-120
Publisher | Google Scholor -
Ajala OA, Sanni L, Adeyinka SA. Accessibility to Health Care Facilities: A Panacea for Sustainable Rural Development in Osun State Southwestern, Nigeria. J Hum Ecol. 2005 Oct;18(2):121–8. DOI: 10.1080/09709274.2005.11905819
Publisher | Google Scholor -
Anka Nasiru M, Abubakar U. Perceived Influence of Transportation on Health-seeking Behavior among Obstetric Fistula Patients in Nigeria: A qualitative Study. Nurs Health Sci. 2019 Dec 5;8:53–8. DOI: 10.9790/1959-0806055358
--> -
Taheri P, Butz D, Greenfield L. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000 Sep 1;191:123–30. DOI: 10.1016/s1072-7515(00)00352-5
Publisher | Google Scholor -
Ikenna K, Gomam M, Emmanuel N. An evaluation of the national health insurance scheme (NHIS) in Jos, a north-central Nigerian city. http://garj.org/garjm/index.htm
--> -
Kofoworola AA, Ekiye A, Motunrayo A, Adeoye T, Adunni M. National Health Insurance Scheme: An Assessment of Service Quality and Clients’ Dissatisfaction. Ethiop J Health Sciemce. 2020;30(5):796–802. DOI: 10.4314/ejhs.v30i5.20
Publisher | Google Scholor -
Irene C, Komomo EA, Agada PO, Augustina OO, Asuquo EO. The Barriers to Accessibility and Availability of Essential Drugs in Public and Private Health Facilities in Calabar Metropolis, Cross River State, Nigeria. J Health Med Nurs. 2016;27. Corpus ID: 54704277
Publisher | Google Scholor -
Ofoli JNT, Ashau-Oladipo T, Hati SS, Ati L, Ede V. Preventive healthcare uptake in private hospitals in Nigeria: A cross-sectional survey (Nisa premier hospital). BMC Health Serv Res. 2020;20(1):1–10. DOI: https://doi.org/10.1186/s12913-020-05117-5
Publisher | Google Scholor -
Ibrahim N, Pozo-Martin F, Gilbert C. Direct non-medical costs double the total direct costs to patients undergoing cataract surgery in Zamfara state, Northern Nigeria: a case series. BMC Health Serv Res. 2015 Apr 16;15(1):163. DOI: 10.1186/s12913-015-0831-2
Publisher | Google Scholor -
Alege PO, Oye QE, Ogundipe A, Adu O. Macroeconomic Effect Of Minimum Wage Increase In Nigeria: A DSGE Approach. Niger J Econ Soc Stud. 2021;63(2):271–99. https://eprints.covenantuniversity.edu.ng/15052/
Publisher | Google Scholor -
World Bank. Poverty & Equity Brief. 2021. https://www.worldbank.org/en/topic/poverty/publication/poverty-and-equity-briefs
Publisher | Google Scholor -
Adegboyega O, Abioye K. Effects of Health-Care Services and Commodities Cost on the Patients at the Primary Health Facilities in Zaria Metropolis, North Western Nigeria. Niger J Clin Pract. 2017 Aug;20(8):1027. DOI: 10.4103/njcp.njcp_61_16
Publisher | Google Scholor -
Adewole DA, Dairo MD, Bolarinwa OA. Awareness and Coverage of the National Health Insurance Scheme among Formal Sector Workers in Ilorin, Nigeria. AfrJBiomedRes. 2016;19. DOI: 10.9734/IJTDH/2016/27777
Publisher | Google Scholor -
Ibadin MO, Akpede GO. A revised scoring scheme for the classification of socio-economic status in Nigeria. Nigerian Journal of Paediatrics. 2021 Feb 4;48(1):26-33. DOI:10.4314/njp.v48i1.5
Publisher | Google Scholor -
2Ogaji DS, Nwi-ue LB, Agalah HN, Ibok SG, N-ue DM. Impact and contributors to cost of managing long term conditions in a university hospital in Nigeria. J Community Med Prim Health Care. 2015;27(2):30–40. Corpus ID: 79006762
Publisher | Google Scholor -
Aregbeshola, B. S., & Khan, S. M. Original Article Out-of-Pocket Payments, Catastrophic Health Expenditure and Poverty Among Households in Nigeria. Int J. Health Policy Manag, 2018 7(9), 798–806. https://DOI.org/10.15171/ijhpm.2018.19
Publisher | Google Scholor -
https://www.un-ilibrary.org/docserver/fulltext/27081990/10.18356/27081990-107/27081990-107-en_web.pdf
--> -
World Bank. Poverty and Equity brief-Saharan Africa. 2020. Page 1 https://databankfiles.worldbank.org/data/download/poverty/33EF03BB-9722-4AE2-ABC7-AA2972D68AFE/Global_POVEQ_SDN.pdf.
-->
